Optimizing Surgical Prophylaxis: An Audit of Antibiotic Use and Guideline Adherence in a Tertiary Care Hospital with Focus on Antimicrobial Stewardship
Abstract
 Abstract Views: 0
Abstract Views: 0
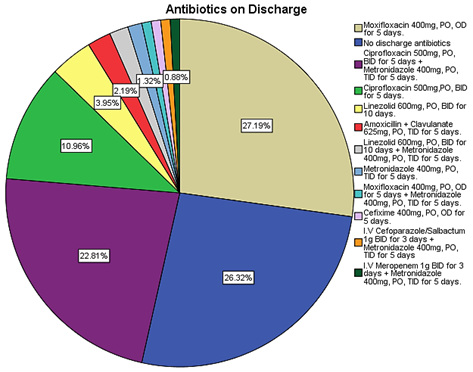
Inappropriate antibiotic use, particularly in surgical prophylaxis, contributes to increasing antibiotic resistance and surgical site infections (SSIs). This study aimed to evaluate pre- and post-operative antibiotic prescribing practices and compliance with surgical prophylaxis guidelines in a tertiary care hospital, identifying areas for antimicrobial stewardship (AMS) intervention. A prospective study was conducted, collecting data on 250 surgical patients. After excluding 6 patients based on pre-defined criteria, data from 244 patients was analyzed using SPSS 20.0. The audit assessed patient demographics, pre- and post-operative antibiotic regimens, duration of antibiotic administration, and incidence of SSIs. Analysis revealed widespread use of broad-spectrum antibiotics for surgical prophylaxis, often deviating from established guidelines. Intravenous (IV) antibiotics were commonly administered for extended durations (24–72 hours) post-operatively. A significant proportion of patients (n=167) received oral antibiotics upon discharge to complete a 5-day course. The SSI incidence rate was 2.0%, with all infections occurring in patients who underwent open surgical procedures (laparotomies). Staphylococcus aureus was the most frequently isolated organism (including methicillin-resistant strains), followed by Klebsiella pneumoniae and Escherichia coli. Most isolates exhibited multidrug resistance, although they remained sensitive to antibiotics, such as vancomycin, linezolid, meropenem, and colistin. Management was guided by culture and sensitivity in most cases; however, one instance of irrational antibiotic use was observed. These findings emphasize the role of surgical type, duration, and appropriate microbial management in SSI prevention. In conclusion, the study highlighted significant deviations from surgical prophylaxis guidelines and irrational antibiotic use. The presence of multidrug-resistant organisms (MDROs) and inappropriate antibiotic selection further stressed the urgent need for targeted AMS interventions. These should include the development and implementation of hospital-specific prophylaxis protocols aligned with the best national or international practices. Ongoing monitoring is needed to assess AMS effectiveness.
Downloads
References
Kourbeti I, Aikaterini K, Michael S. Antibiotic stewardship in surgical departments. Antibiotics (Basel). 2024;13(4):e329. https://doi.org/10.3390/antibiotics13040329
Gautam S, Simranpreet K. Revolutionizing biomedicine: metal-organic frameworks combating multi-drug resistance. Mater Lett. 2024;354:e135306. https://doi.org/10.1016/j.matlet.2023.135306
Perez KK, Drake TC, Fuentes A, Gentry CN. 1095. Prevalence and characteristics of self-reported antibiotic allergies across a multi-hospital healthcare system. Open Forum Infect Dis. 2019;6(Suppl 2):S389–S390. https://doi.org/10.1093/ofid/ofz360.959
Seah XFV. 69. Impact of antimicrobial stewardship interventions on post-elective caesarean antibiotic prophylaxis and surgical site infections. Open Forum Infect Dis. 2020;7(Suppl 1):eS53. https://doi.org/10.1093/ofid/ofaa439.114
Hickman K, Nicolas F, Mandelin C, Shivanne B, Brandy R. Implementing a health-system–wide antibiotic stewardship program in ambulatory surgery centers. Antimicrob Steward Healthc Epidemiol. 2023;3(S2):s2–s27. https://doi.org/10.1017/ash.2023.250
Giordano M, Lorena S, Maria P. Appropriateness of surgical antibiotic prophylaxis in pediatric patients in Italy. Infect Control Hosp Epidemiol. 2017;38(7):823–831. https://doi.org/10.1017/ice.2017.79
Brink AJ, Messina AP, Feldman C, Richards GA, van den Bergh D. From guidelines to practice: a pharmacist-driven prospective audit and feedback improvement model for peri-operative antibiotic prophylaxis in 34 South African hospitals. J Antimicrob Chemother. 2017;72(4):1227–1234. https://doi.org/10.1093/jac/dkw523
Sharma R, Dinesh L. Acinetobacter baumannii: a comprehensive review of global epidemiology, clinical implications, host interactions, mechanisms of antimicrobial resistance and mitigation strategies. Microb Pathog. 2025;204:e107605. https://doi.org/10.1016/j.micpath.2025.107605
Jerome JTJ, Arun K, Mauli C. Surgical management for distal phalanx osteomyelitis: a narrative review. J Clin Orthop Trauma. 2025;66:e103021. https://doi.org/10.1016/j.jcot.2025.103021
Simoni A, Laura S, Guillermo YJ, Christina BC, John DS. Current and emerging strategies to curb antibiotic-resistant urinary tract infections. Nat Rev Urol. 2024;21(12):1–16. https://doi.org/10.1038/s41585-024-00877-9
Mzumara GW, Michael M, Pui-Ying IT. Protocols, policies and practices for antimicrobial stewardship in hospitalized patients in least-developed and low-income countries: a systematic review. Antimicrob Resist Infect Control. 2023;12(1):e131. https://doi.org/10.1186/s13756-023-01335-8
Zwicky SN, Severin G, Franziska T, et al. No impact of sex on surgical site infections in abdominal surgery: a multi-center study. Langenbecks Arch Surg. 2022;407(8):3763–3769. https://doi.org/10.1007/s00423-022-02691-6
Iqbal S, Iftikhar M, Qureshi HU, Khan AG, Ullah S. Frequency of surgical site infection after appendicectomy. J Peoples Univ Med Health Sci Nawab. 2024;14(3):32–37. http://doi.org/10.46536/jpumhs/2024/14.03.532
Bucataru A, Maria B, Alice EG, et al. Factors contributing to surgical site infections: a comprehensive systematic review of etiology and risk factors. Clin Pract. 2023;14(1):52–68. http://doi.org/10.3390/clinpract14010006
Li H, Xufeng Z, Jie G. Extensive analysis of risk factors associated with surgical site infections post‐cardiothoracic open surgery. Int Wound J. 2024;21(3):e14842. https://doi.org/10.1111/iwj.14842
Zhang L, Er-Nan L. Risk factors for surgical site infection following lumbar spinal surgery: a meta-analysis. Ther Clin Risk Manag. 2018;14:2161–2169. https://doi.org/10.2147/TCRM.S181477
Chola B. Evaluation of The Compliance of Antibiotic Prescribing with International Clinical Practice Guidelines for Surgical Antibiotic Prophylaxis at Intermediate Hospital Rundu, Namibia [dissertation]. Windhoek: University of Namibia; 2022.
Hyland SJ. Perioperative antimicrobial stewardship and pharmacy’s role. https://ce.pharmacy.premierinc.com/assets/ClientID_168/EventAssets/perioperative-abx-stewardship-hs-handout.pdf. Updated May 6, 2023. Accessed January 15, 2025.
Kelley WE Jr. The evolution of laparoscopy and the revolution in surgery in the decade of the 1990s. J Soc Laparoendosc Surg. 2008;12(4):351–357.
Alkatout I, Ulrich M, Liselotte M, et al. The development of laparoscopy—a historical overview. Front Surg. 2021;8:e799442. https://doi.org/10.3389/fsurg.2021.799442
Wang SH. Evaluating risk factors for surgical site infections and the effectiveness of prophylactic antibiotics in patients undergoing laparoscopic cholecystectomy. World J Gastrointest Surg. 2025;17(1):e98567. https://doi.org/10.4240/wjgs.v17.i1.98567
Muhamad AN, Cindy SJT, Mohd RD, et al. High incidence of multidrug-resistant organisms and modifiable risk factors associated with surgical site infections: A cohort study in a tertiary medical center in Kuala Lumpur, Malaysia from 2020 to 2023. Antimicrob Resist Infect Control. 2025;14(1):e22. https://doi.org/10.1186/s13756-025-01537-2
World Health Organization. Global report on infection prevention and control 2024. https://www.who.int/publications/i/item/9789240103986. Updated November 29, 2024. Accessed January 16, 2025.
Hoffman T, Shitrit P, Chowers M. Risk factors for surgical site infections following open versus laparoscopic colectomies: a cohort study. BMC Surg. 2021;21:e376. https://doi.org/10.1186/s12893-021-01379-w
Cheng H, Brian PHC, Ireena MS, Nicole CF, Chris GC, Piet H. Prolonged operative duration increases risk of surgical site infections: a systematic review. Surgical Infect. 2017;18(6):722–735. https://doi.org/10.1089/sur.2017.089
Afifi IK, Eman AL, Khalil MA. Surgical site infections after elective general surgery in Tanta University Hospital: Rate, risk factors and microbiological profile. Egyp J Med Microbiol. 2009;18(2):61–72.
Mundhada AS, Sunita T. A study of organisms causing surgical site infections and their antimicrobial susceptibility in a tertiary care government hospital. Indian J Pathol Microbiol. 2015;58(2):195–200. https://doi.org/10.4103/0377-4929.155313
Iqbal R, Palwasha A, Zumaira T. Antimicrobial susceptibility pattern of pathogens isolated from surgical wound infections in tertiary care hospitals of Pakistan. Afr Health Sci. 2025;25(1):1–11.
Nimkar P, Kanyal D. Understanding the financial burden of surgical site infections: A narrative review. Multidiscip Rev. 2025;8(3):e2025084. https://doi.org/10.31893/multirev.2025084
Liu H, Xing H, Zhang G, Wei A, Chang Z. Risk factors for surgical site infections after orthopaedic surgery: a meta‐analysis and systematic review. Int Wound J. 2025;22(5):e70068. https://doi.org/10.1111/iwj.70068
Karnwal A, Jassim AY, Mohammed AA, Al-Tawaha ARMS, Selvaraj M, Malik T. Addressing the global challenge of bacterial drug resistance: Insights, strategies, and future directions. Front Microbiol. 2025;16:e1517772. https://doi.org/10.3389/fmicb.2025.1517772
Rosa WE, Pandey S, Wisniewski R, et al. Antimicrobials in serious illness and end-of-life care: lifting the veil of silence. Lancet Infect Dis. 2025;25:e416-e431. https://doi.org/10.1016/S1473-3099(24)00832-6
Hassan A, Rehman NU, Maqbool S, Arif M. Pharmacist-led antibiotic interventions in infectious disease patients: a Pakistani tertiary care antimicrobial stewardship study. J Pharm Policy Pract. 2025;18(1):e2450017. https://doi.org/10.1080/20523211.2025.2450017
Bwire GM, Magati RB, Ntissi HH, et al. Synthesizing evidence to guide the design and implementation of effective strategies for discontinuing postoperative antibiotic prophylaxis in surgical settings: an umbrella review post-WHO 2018 recommendations. Syst Rev. 2025;14(1):e7. https://doi.org/10.1186/s13643-024-02750-7
Paganetti C, Subotic U, Sanchez C, et al. Implementation of surgical site infection prophylaxis in children–a cross sectional prospective study. J Hosp Infect. Published online May 6, 2025. https://doi.org/10.1016/j.jhin.2025.03.018
Copyright (c) 2025 Junaid Naeem, Sajid Khan Sadozai, Saeed Ahmad Khan, Syed Majid Shah, Sajid Hussain, Majid Khan Sadozai, Farina Kanwal, Naveed Safdar

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution (CC-BY) 4.0 License that allows others to share the work with an acknowledgement of the work’s authorship and initial publication in this journal