Cost-Effectiveness Analysis of Antihypertensive Medications Prescribed to Primary Hypertension Patients at District Headquarters Hospital, Kohat
Abstract
 Abstract Views: 0
Abstract Views: 0
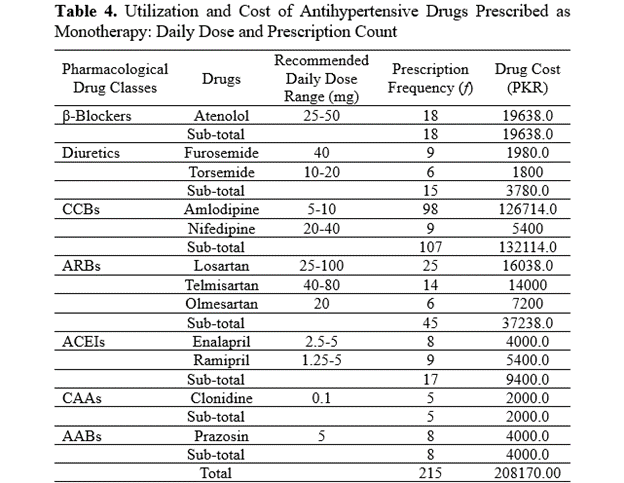
Hypertension, a major risk factor for cardiovascular diseases (CVDs), contributes to 9.3 million deaths annually. In low- and middle-income countries (LMICs) like Pakistan, cost-effective treatment is critical due to limited healthcare resources. This study aimed to evaluate the cost-effectiveness of antihypertensive medications prescribed to patients with primary hypertension at the District Headquarters (DHQ) Hospital, KDA, Kohat in the Khyber Pakhtunkhwa province of Pakistan. A cross-sectional retrospective study was conducted over a period of six months, involving 320 patients (55.31% male, 44.69% female) aged 18-60 years. Prescription patterns and costs of antihypertensive medications (monotherapy and combination therapy) were analyzed using hospital records. The total cost of prescribed antihypertensive medications was PKR 261,153.00, with monotherapy accounting for PKR 208170.00 and combination therapy accounting for PKR 52983.00. Among monotherapies, calcium channel blockers (CCBs) were the most frequently prescribed (107 prescriptions) and accounted for the highest cost (PKR 132114.00, 50.58%), followed by angiotensin receptor blockers (ARBs) (PKR 37238.00, 14.25%). In contrast, diuretics were the most cost-effective option, costing only PKR 25.2 per unit dose. For combination therapy, amlodipine + hydrochlorothiazide combination was the most prescribed, while losartan + amlodipine combination incurred the highest cost. Monotherapy was prescribed in 67.18% of cases, with most patients showing a positive response before transitioning to combination therapy. CCBs and diuretics were found to be more cost-effective, whereas ACE inhibitors were among the most expensive options. CCBs were the most frequently prescribed in monotherapy, while the combination of amlodipine and atenolol was commonly used in multidrug regimens. The current study highlights the importance of considering patients’ socioeconomic status when initiating pharmacologic treatment. Cost-effective prescribing is crucial in the resource-limited settings of Pakistan, where balancing clinical efficacy and affordability is essential. The findings support WHO recommendations for the rational use of combination therapy and emphasize the use of low-cost medications to optimize treatment outcomes in low- and middle-income countries.
Downloads
References
Carey RM, Wright JT, Taler SJ, Whelton PK. Guideline-driven management of hypertension: an evidence-based update. Circ Res. 2021;128(7):827–846. https://doi.org/10.1161/CIRCRESAHA.121.318083
James PA, Oparil S, Carter BL, et al. Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. https://doi.org/10.1001/jama.2013.284427
Dixon DL, Johnston K, Patterson J, Marra CA, Tsuyuki RT. Cost-effectiveness of pharmacist prescribing for managing hypertension in the United States. JAMA Net Open. 2023;6(11):e2341408. https://doi.org/10.1001/jamanetworkopen.2023.41408
Jafari A, Mirbehbahani SH, Golestani A, et al. Cardiometabolic risk factors trend in Iranian adults with hypertension over 15 years: findings of nationwide steps of 2007–2021. J Diabetes Metab Disord. 2024;23:2315–2328. https://doi.org/10.1007/s40200-024-01498-0
Arshad V, Samad Z, Das J, et al. Prescribing patterns of antihypertensive medications in low-and middle-income countries: a systematic review. Asia Pac J Public Health. 2021;33(1):14–22. https://doi.org/10.1177/1010539520965280
Schutte AE, Venkateshmurthy NS, Mohan S, Prabhakaran D. Hypertension in low-and middle-income countries. Circ Res. 2021;128(7):808–826. https://doi.org/10.1161/CIRCRESAHA.120.318729
Whelton WP. Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2017;71(9):e129.
Elahi A, Ali AA, Khan AH, et al. Challenges of managing hypertension in Pakistan-a review. Clin Hypertens. 2023;29:e17. https://doi.org/10.1186/s40885-023-00245-6
Godman B, Fadare J, Kwon HY, et al. Evidence-based public policy making for medicines across countries: findings and implications for the future. J Comp Eff Res. 2021;10(12):1019–1052. https://doi.org/10.2217/cer-2020-0273
Virani SS, Newby L, Arnold S, et al. Guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2023;82(9):833–955. https://doi.org/10.1016/j.jacc.2023.04.003
Ojha U, Ruddaraju S, Sabapathy N, et al. Current and emerging classes of pharmacological agents for the management of hypertension. Am J Cardiovasc Drugs. 2022;22:1–15. https://doi.org/10.1007/s40256-021-00510-9
Tiet N. Self-Monitoring Blood Pressure as A Tool in the Primary Care Setting [dissertation]. The University of Arizona; 2022.
Roberts MH, Ferguson GT. Real-world evidence: bridging gaps in evidence to guide payer decisions. PharmacoEconomics Open. 2021;5:3–11. https://doi.org/10.1007/s41669-020-00221-y
Poluzzi E, Petrović A, Wettermark B. Drug utilization research on cardiovascular medicines. In: Elseviers M, Wettermark B, Benkó R, et al. eds. Drug Utilization Research. Wiley Publishers; 2024:332–341. https://doi.org/10.1002/9781119911685.ch32
Sun Z, Zhang H, Ding Y, et al. Cost-Effectiveness of salt substitution and antihypertensive drug treatment in Chinese prehypertensive adults. Hypertension. 2024;81(12):2529–2539. https://doi.org/10.1161/HYPERTENSIONAHA.124.23412
Cao S, Chatterjee C. Equilibrium effects of pharmaceutical bundling: evidence from India. SSRN. 2022. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4037548
Iqbal MA, Adil M, Khalil A, Hassan Z, Faraz N, Khan M. Profile and etiology of hypertensive patients at young age in Pakistani population. Rawal Med J. 2022;47(4):872–875.
Al-Makki A, DiPette D, Whelton PK, et al. Hypertension pharmacological treatment in adults: a World Health Organization guideline executive summary. Hypertension. 2022;79(1):293–301. https://doi.org/10.1161/HYPERTENSIONAHA.121.18192
Jeemon P, Séverin T, Amodeo C, et al. World heart federation roadmap for hypertension–a 2021 update. Glob Heart. 2021;16(1):e63. https://doi.org/10.5334/gh.1066
Beshah SA, Husain MJ, Dessie GA, et al. Cost analysis of the WHO-HEARTS program for hypertension control and CVD prevention in primary health facilities in Ethiopia. Public Health Pract. 2023;6:e100423. https://doi.org/10.1016/j.puhip.2023.100423
Riaz M, Shah G, Asif M, Shah A, Adhikari K, Abu-Shaheen A. Factors associated with hypertension in Pakistan: a systematic review and meta-analysis. PloS-One. 2021;16(1):e0246085. https://doi.org/10.1371/journal.pone.0246085
Fatima H, Fatima N, Ahmad S, Ahmad H, Sheikh N. Prevalence and risk factors of hypertension in young adults and middle-aged individuals: a cross-sectional study. Albus Scientia. 2024;2:1–3. https://doi.org/10.56512/as.2024.2.e241223
Wang JG, Palmer BF, Vogel Anderson K, Sever P. Amlodipine in the current management of hypertension. J Clin Hypertens. 2023;25(9):801–807. https://doi.org/10.1111/jch.14709
Sharma D, Mehta DK, Bhatti K, Das R, Chidurala RM. Amlodipine and atenolol: combination therapy versus monotherapy in reducing blood pressure-A focus on safety and efficacy. Res J Pharm Technol. 2020;13(6):3007–3013.
Sturdivant T, Allen-Thomas K. ACE inhibitors and ARBs: understanding the basics. Nurs Made Incred Easy. 2023;21(1):14–21. https://doi.org/10.1097/01.NME.0000899392.70376.a2
Escudero VJ, Mercadal J, Molina-Andújar A, et al. New insights into diuretic use to treat congestion in the ICU: beyond furosemide. Front Nephrol. 2022;2:e879766. https://doi.org/10.3389/fneph.2022.879766
Akhter MS, Ahmad HB. Recent advances in therapeutic approach for hypertension to improve cardiac health. In: Tombak A, ed. Hemodynamics of the Human Body. Intech Open; 2024. https://doi.org/10.5772/intechopen.111841
Karunarathna I, Kusumarathna K, Jayathilaka P, Withanage C. Comprehensive Management of Hypertension: Strategies, Guidelines, and Emerging Therapies. Uva Clinical Lab; 2024.
Lauder L, Mahfoud F, Azizi M, et al. Hypertension management in patients with cardiovascular comorbidities. Eur Heart J. 2023;44(23):2066–2077. https://doi.org/10.1093/eurheartj/ehac395
Sharma H, Kumar A, Kaur S, Singh J, Sharma G. Cost analysis of oral antihypertensive drugs: assessing the effect of drug price control order in India. Asian J Pharm Clin Res. 2022;15(9):73–76. http://dx.doi.org/10.22159/ajpcr.2022v15i9.46092.
Davari M, Kebriaeezadeh A, Sorato MM, Soleymani F. Impact of fixed dose combination treatment on adherence, blood pressure control, clinical outcomes and cost of treatment. J PharmacoEcon Pharm Manage. 2022;8(3):1–14.
An J, Ni L, Mefford MT, et al. EE222 Healthcare costs associated with initial combination therapy versus monotherapy for patients with hypertension. Value Health. 2023;26(6):S99–S100. https://doi.org/10.1016/j.jval.2023.03.523
McNally RJ, Morselli F, Farukh B, Chowienczyk PJ, Faconti, L. A review of the prescribing trend of thiazide‐type and thiazide‐like diuretics in hypertension: a UK perspective. Br J Clin Pharmacol. 2019;85(12):2707–2713. https://doi.org/10.1111/bcp.14109
Zhu J, Chen N, Zhou M, et al. Calcium channel blockers versus other classes of drugs for hypertension. Cochrane Database Syst Rev. 2021;(10):eCD003654. https://doi.org/10.1002/14651858.CD003654
Kovács B, Darida M, Simon J. Drugs becoming generics—the impact of genericization on the market performance of antihypertensive active pharmaceutical ingredients. Int J Environ Res Public Health. 2021;18(18):e9429. https://doi.org/10.3390/ijerph18189429
Ashraf T, Aamir KF, Nadeem A, et al. Impact of educational intervention on hypertension management by primary care physician: a randomized control trial. PEC Innov. 2024;4:e100285. https://doi.org/10.1016/j.pecinn.2024.100285
Kučan M, Lulić I, Pelčić JM, Mozetič V, Vitezić D. Cost effectiveness of antihypertensive drugs and treatment guidelines. Eur J Clin Pharmacol. 2021;77(11):1665–1672. https://doi.org/10.1007/s00228-021-03163-4
Copyright (c) 2025 Marvi Shaheen, Sajid Khan Sadozai, Rooh Ullah, Sajid Hussain, Fawad Ali, Majid Khan Sadozai, Farina Kanwal, Naveed Safdar

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution (CC-BY) 4.0 License that allows others to share the work with an acknowledgement of the work’s authorship and initial publication in this journal