Reducing Multidrug-Resistant (MDR) Klebsiella pneumoniae via the Efficient Use of Bacteriophages ZI3 and HI3
Abstract
 Abstract Views: 0
Abstract Views: 0
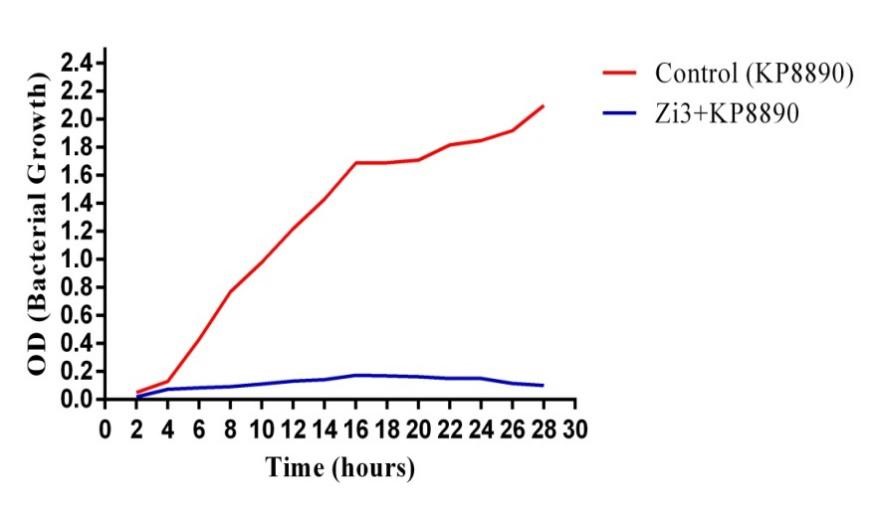
Klebsiella pneumoniae is a common cause of multidrug-resistant (MDR) pneumonia, bacteremia, urinary tract infections (UTIs), and other systemic infections. K. pneumoniae is the third most common pathogen in blood cultures from sepsis patients. It can cause severe epidemic and endemic nosocomial infections. Antibiotic treatment of K. pneumoniae infections is getting increasingly challenging due to the development of antimicrobial resistance among pathogens. Hence, a new alternative strategy is required to treat such infections. Bacteriophages are the most prevalent biological entity on the planet with an estimated 1031 particles. As obligatory intracellular parasites, they infect bacterial cells. They have a high host specificity and can replicate and lyse bacterial cells. In this research, two novel indigenous bacteriophages against K. pneumoniae strain kp8890 were isolated, characterized, and labeled as ZI3 and HI3. Both these phages were found to have a specific host range for K. pneumoniae. HI3 was able to lyse 7 out of 10 different K. pneumoniae clinical isolates, while ZI3 was able to lyse 5 out of 10 isolates, although it could not infect bacteria from other species. The isolated phages showed viability up to 50°C and pH ranging from 3 to 9. HI3 inhibited bacterial growth for 18 hours. Whereas, ZI3 showed an excellent bacterial reduction ability by inhibiting and decreasing the number of initial bacterial inoculum for 24 hours of observation. Keeping in view the excellent bacterial growth reduction, phage titer, pH and thermal stability, and host range, it is suggested that both bacteriophages, that is, ZI3 and HI3 can be potential phage therapy candidates after necessary animal modeling and clinical trials in the future.
Downloads
Copyright (c) 2023 Zia Ullah, Iqbal Ahmad Alvi, Zeeshan Niaz, Iftikhar Ullah, Atta Ullah, Shafiq Ur Rehman

This work is licensed under a Creative Commons Attribution 4.0 International License.
Author(s) retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution (CC-BY) 4.0 License that allows others to share the work with an acknowledgment of the work’s authorship and initial publication in this journal.