Anophthalmia and Microphthalmia in Pakistan: Current Genetic Insights and Future Perspectives
Abstract
 Abstract Views: 0
Abstract Views: 0
Anophthalmia and microphthalmia (A/M) are genetic disorders characterized by the absence or reduced size of the ocular globe, as compared to the globe size of the normal population. These disorders can be inherited in both autosomal recessive and dominant patterns. Certain genes have been reported to contribute significantly to the emergence of diseased phenotypes. Mutation in Forkhead Box E3 gene has been reported in different studies involving the Pakistani population, where the pattern of inheritance is autosomal recessive. Moreover, ALDH1A3 and VSX2 have been associated as well with severe phenotypes of A/M. SOX2 has been reported in the cases of de novo mutations and syndromic microphthalmia. The current review summarizes the most recurrent mutations in these genes in patients suffering from A/M in Pakistan. It showcases the importance of variant studies and how the demographic location of individuals may make them susceptible to a particular type of mutation. It also compares mutation profiles between the Pakistani population and global cohorts, emphasizing the impact of consanguineous marriages on the high prevalence of these conditions in the country. More studies may prove helpful in formulating a diagnostic kit for this disease so that a genotype-phenotype correlation can be established.
Downloads
References
von der Lippe C, Neteland I, Feragen KB. Children with a rare congenital genetic disorder: a systematic review of parent experiences. Orphanet J Rare Dis. 2022;17:e375. https://doi.org/10.1186/s13023-022-02525-0
Chassaing N, Causse A, Vigouroux A, et al. Molecular findings and clinical data in a cohort of 150 patients with anophthalmia/microphthalmia. Clin Genet. 2014;86(4):326–334. https://doi.org/10.1111/cge.12275
Slavotinek AM. Genetics of anophthalmia and microphthalmia. Part 2: syndromes associated with anophthalmia–microphthalmia. Hum Genet. 2019;138:831–846. https://doi.org/10.1007/s00439-018-1949-1
Verma AS, FitzPatrick DR. Anophthalmia and microphthalmia. Orphanet J Rare Dis. 2007;2:e47. https://doi.org/10.1186/1750-1172-2-47
Stoll C, Dott B, Alembik Y, Roth M-P. Associated anomalies in anophthalmia and microphthalmia. Eur J Med Genet. 2024;67:e104892. https://doi.org/10.1016/j.ejmg.2023.104892
Richardson R, Sowden J, Gerth-Kahlert C, Moore AT, Moosajee M. Clinical utility gene card for: non-syndromic microphthalmia including next-generation sequencing-based approaches. Eur J Hum Genet. 2017;25:e512. https://doi.org/10.1038/ejhg.2016.201
Williamson KA, FitzPatrick DR. The genetic architecture of microphthalmia, anophthalmia and coloboma. Eur J Medi Genet. 2014;57(8):369–380. https://doi.org/10.1016/j.ejmg.2014.05.002
Overk CR, Cartier A, Shaked G, et al. Hippocampal neuronal cells that accumulate α-synuclein fragments are more vulnerable to Aβ oligomer toxicity via mGluR5–implications for dementia with Lewy bodies. Mol Neurodegeneration. 2014;9:e18. https://doi.org/10.1186/1750-1326-9-18
Gregory-Evans C, Williams M, Halford S, Gregory-Evans K. Ocular coloboma: a reassessment in the age of molecular neuroscience. J Med Genet. 2004;41:881–891. https://doi.org/10.1136/jmg.2004.025494
Shah SP, Taylor AE, Sowden JC, et al. Anophthalmos, microphthalmos, and typical coloboma in the United Kingdom: a prospective study of incidence and risk. Invest Ophthalmol Vis Sci. 2011;52:558–564. https://doi.org/10.1167/iovs.10-5263
Bernstein CS, Anderson MT, Gohel C, Slater K, Gross JM, Agarwala S. The cellular bases of choroid fissure formation and closure. Dev Biol. 2018;440(2):137–151. https://doi.org/10.1016/j.ydbio.2018.05.010
Casey J, Kawaguchi R, Morrissey M, et al. First implication of STRA6 mutations in isolated anophthalmia, microphthalmia, and coloboma: a new dimension to the STRA6 phenotype. Hum Mutat. 2011;32(12):1417–1426. https://doi.org/10.1002/humu.21590
Slavotinek AM. Eye development genes and known syndromes. Mol Genet Metabol. 2011;104(4):448–456. https://doi.org/10.1016/j.ymgme.2011.09.029
Schneider A, Bardakjian T, Reis LM, Tyler RC, Semina EV. Novel SOX2 mutations and genotype–phenotype correlation in anophthalmia and microphthalmia. Am J Med Genet Part A. 2009;149A:2706–2715. https://doi.org/10.1002/ajmg.a.33098
Plaisancié J, Ceroni F, Holt R, et al. Genetics of anophthalmia and microphthalmia. Part 1: non-syndromic anophthalmia/microphthalmia. Hum Genet. 2019;138:799–830. https://doi.org/10.1007/s00439-019-01977-y
Givens KT, Lee DA, Jones T, Ilstrup DM. Congenital rubella syndrome: ophthalmic manifestations and associated systemic disorders. Br J Ophthalmol. 1993;77(6):358–363. https://doi.org/10.1136/bjo.77.6.358
Busby A, Dolk H, Armstrong B. Eye anomalies: seasonal variation and maternal viral infections. Epidemiology. 2005;16(3):317–322. https://doi.org/10.1097/01.ede.0000158817.43037.ab
Slavotinek AM, Garcia ST, Chandratillake G, et al. Exome sequencing in 32 patients with anophthalmia/microphthalmia and developmental eye defects. Clin Genet. 2015;88(5):468–473. https://doi.org/10.1111/cge.12543
Blixt Å, Mahlapuu M, Aitola M, Pelto-Huikko M, Enerbäck S, Carlsson P. A forkhead gene, FoxE3, is essential for lens epithelial proliferation and closure of the lens vesicle. Gen Dev. 2000;14:245–254. https://doi.org/10.1101/gad.14.2.245
Brownell I, Dirksen M, Jamrich M. Forkhead Foxe3 maps to the dysgenetic lens locus and is critical in lens development and differentiation. Genesis. 2000;27(2):81–93. https://doi.org/10.1002/1526-968x(200006)27:2%3C81::aid-gene50%3E3.0.co;2-n
Semina EV, Brownell I, Mintz-Hittner HA, Murray JC, Jamrich M. Mutations in the human forkhead transcription factor FOXE3 associated with anterior segment ocular dysgenesis and cataracts. Hum Mol Genet. 2001;10(3):231–236. https://doi.org/10.1093/hmg/10.3.231
Ormestad M, Blixt As, Churchill A, Martinsson T, Enerbäck S, Carlsson P. Foxe3 haploinsufficiency in mice: a model for Peters’ anomaly. Invest Ophthalmol Vis Sci. 2002;43(5):1350–1357.
Reis LM, Sorokina EA, Dudakova L, et al. Comprehensive phenotypic and functional analysis of dominant and recessive FOXE3 alleles in ocular developmental disorders. Hum Mol Geneti. 2021;30(17):1591–1606. https://doi.org/10.1093/hmg/ddab142
Holbrook JA, Neu-Yilik G, Hentze MW, Kulozik AE. Nonsense-mediated decay approaches the clinic. Nat Genet. 2004;36:801–808. https://doi.org/10.1038/ng1403
Valleix S, Niel F, Nedelec B, et al. Homozygous nonsense mutation in the FOXE3 gene as a cause of congenital primary aphakia in humans. Am J Hum Genet. 2006;79(2):358–364. https://doi.org/10.1086/505654
Blixt Å, Landgren H, Johansson BR, Carlsson P. Foxe3 is required for morphogenesis and differentiation of the anterior segment of the eye and is sensitive to Pax6 gene dosage. Dev Biol. 2007;302(1):218–229. https://doi.org/10.1016/j.ydbio.2006.09.021
Shi X, Luo Y, Howley S, et al. Zebrafish foxe3: roles in ocular lens morphogenesis through interaction with pitx3. Mech Dev. 2006;123(10):761–782. https://doi.org/10.1016/j.mod.2006.07.004
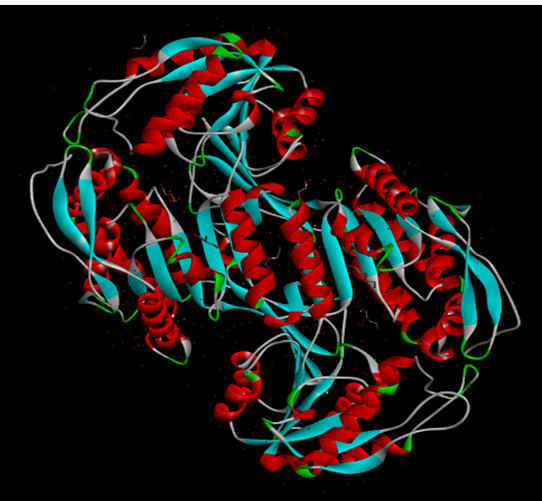
Jumper J, Evans R, Pritzel A, et al. Highly accurate protein structure prediction with AlphaFold. Nature. 2021;596(7873):583–589. https://doi.org/10.1038/s41586-021-03819-2
Ramirez‐Botero AF, Pachajoa H. Syndromic microphthalmia‐3 caused by a mutation on gene SOX2 in a Colombian male patient. Congen Anom. 2016;56(6):250–252. https://doi.org/10.1111/cga.12170
Faivre L, Williamson KA, Faber V, et al. Recurrence of SOX2 anophthalmia syndrome with gonosomal mosaicism in a phenotypically normal mother. Am J Med Genet Part A. 2006;140(6):636–639. https://doi.org/10.1002/ajmg.a.31114
Chassaing N, Gilbert‐Dussardier B, Nicot F, et al. Germinal mosaicism and familial recurrence of a SOX2 mutation with highly variable phenotypic expression extending from AEG syndrome to absence of ocular involvement. Am J Med Genet Part A. 2007;143(3):289–291. https://doi.org/10.1002/ajmg.a.31524
Chitayat D, Sroka H, Keating S, et al. The PDAC syndrome (pulmonary hypoplasia/agenesis, diaphragmatic hernia/eventration, anophthalmia/microphthalmia, and cardiac defect) (Spear syndrome, Matthew‐Wood syndrome): Report of eight cases including a living child and further evidence for autosomal recessive inheritance. Am J Med Genet Part A. 2007;143A(12):1268–1281. https://doi.org/10.1002/ajmg.a.31788
Chassaing N, Ragge N, Kariminejad A, et al. Mutation analysis of the STRA6 gene in isolated and non‐isolated anophthalmia/microphthalmia. Clin Genet. 2013;83(3):244–250. https://doi.org/10.1111/j.1399-0004.2012.01904.x
Chassaing N, Golzio C, Odent S, et al. Phenotypic spectrum of STRA6 mutations: from Matthew‐Wood syndrome to non‐lethal anophthalmia. Hum Mutat. 2009;30(5):e673–E681. https://doi.org/10.1002/humu.21023
Zuckerkandl E, Pauling L. Evolutionary divergence and convergence in proteins. Evolv Gen Prot. 1965:97–166. https://doi.org/10.1016/B978-1-4832-2734-4.50017-6
Kawaguchi R, Yu J, Honda J, et al. A membrane receptor for retinol binding protein mediates cellular uptake of vitamin A. Science. 2007;315(5813):820–825. https://doi.org/10.1126/science.1136244
Levin MS. Cellular retinol-binding proteins are determinants of retinol uptake and metabolism in stably transfected Caco-2 cells. J Biol Chem. 1993;268(11):8267–8276. https://doi.org/10.1016/S0021-9258(18)53092-1
Isken A, Golczak M, Oberhauser V, et al. RBP4 disrupts vitamin A uptake homeostasis in a STRA6-deficient animal model for Matthew-Wood syndrome. Cell Metabol. 2008;7(3):258–268. https://doi.org/10.1016/j.cmet.2008.01.009
Fares-Taie L, Gerber S, Chassaing N, et al. ALDH1A3 mutations cause recessive anophthalmia and microphthalmia. Am J Hum Genet. 2013;92(2):265–270. https://doi.org/10.1016/j.ajhg.2012.12.003
Abouzeid H, Favez T, Schmid A, et al. Mutations in ALDH 1 A 3 represent a frequent cause of Microphthalmia/Anophthalmia in consanguineous families. Hum Mutat. 2014;35(8):949–953. https://doi.org/10.1002/humu.22580
Plaisancié J, Brémond-Gignac D, Demeer B, et al. Incomplete penetrance of biallelic ALDH1A3 mutations. Eur J Med Genet. 2016;59(4):215–218. https://doi.org/10.1016/j.ejmg.2016.02.004
Hung SS, Khan S, Lo CY, Hewitt AW, Wong RC. Drug discovery using induced pluripotent stem cell models of neurodegenerative and ocular diseases. Pharmacol Ther. 2017;177:32–43. https://doi.org/10.1016/j.pharmthera.2017.02.026
Semerci CN, Kalay E, Yıldırım C, et al. Novel splice-site and missense mutations in the ALDH1A3 gene underlying autosomal recessive anophthalmia/microphthalmia. Br J Ophthalmol. 2014;98(6):832–840. https://doi.org/10.1136/bjophthalmol-2013-304058
Cvekl A, Wang W-L. Retinoic acid signaling in mammalian eye development. Exp Eye Res. 2009;89(3):280–291. https://doi.org/10.1016/j.exer.2009.04.012
Mic FA, Molotkov A, Molotkova N, Duester G. Raldh2 expression in optic vesicle generates a retinoic acid signal needed for invagination of retina during optic cup formation. Dev Dyn. 2004;231(2):270–277. https://doi.org/10.1002/dvdy.20128
Duester G. Keeping an eye on retinoic acid signaling during eye development. Chem Biol Interact. 2009;178(1-3):178–181. https://doi.org/10.1016/j.cbi.2008.09.004
Dupé V, Matt N, Garnier J-M, Chambon P, Mark M, Ghyselinck NB. A newborn lethal defect due to inactivation of retinaldehyde dehydrogenase type 3 is prevented by maternal retinoic acid treatment. Proc Natl Acad Sci USA. 2003;100(24):14036–14041. https://doi.org/10.1073/pnas.2336223100
Barabino SM, Spada F, Cotelli F, Boncinelli E. Inactivation of the zebrafish homologue of Chx10 by antisense oligonucleotides causes eye malformations similar to the ocular retardation phenotype. Mech Dev. 1997;63(2):133–143. https://doi.org/10.1016/S0925-4773(97)00036-1
Percin EF, Ploder LA, Yu JJ, et al. Human microphthalmia associated with mutations in the retinal homeobox gene CHX10. Nature Genet. 2000;25:397–401. https://doi.org/10.1038/78071
Reis LM, Khan A, Kariminejad A, Ebadi F, Tyler RC, Semina EV. VSX2 mutations in autosomal recessive microphthalmia. Mol Vis. 2011;17:2527–2532.
Iseri SU, Wyatt AW, Nürnberg G, et al. Use of genome-wide SNP homozygosity mapping in small pedigrees to identify new mutations in VSX2 causing recessive microphthalmia and a semidominant inner retinal dystrophy. Hum Genet. 2010;128:51–60. https://doi.org/10.1007/s00439-010-0823-6
Iseri SU, Osborne RJ, Farrall M, et al. Seeing clearly: the dominant and recessive nature of FOXE3 in eye developmental anomalies. Hum Mutat. 2009;30(10):1378–1386. https://doi.org/10.1002/humu.21079
Ullah E, Saqib MAN, Sajid S, et al. Genetic analysis of consanguineous families presenting with congenital ocular defects. Exp Eye Res. 2016;146:163–171. https://doi.org/10.1016/j.exer.2016.03.014
Akbar W, Ullah A, Haider N, et al. Identification of novel homozygous variants in FOXE3 and AP4M1 underlying congenital syndromic anophthalmia and microphthalmia. J Gene Med. 2024;26(1):e3601. https://doi.org/10.1002/jgm.3601
Basharat R, Rodenburg K, Rodríguez-Hidalgo M, et al. Combined single gene testing and genome sequencing as an effective diagnostic approach for Anophthalmia and Microphthalmia patients. Genes. 2023;14(8):e1573. https://doi.org/10.3390/genes14081573
Lin S, Harlalka GV, Hameed A, et al. Novel mutations in ALDH1A3 associated with autosomal recessive anophthalmia/microphthalmia, and review of the literature. BMC Med Genet. 2018;19:e160. https://doi.org/10.1186/s12881-018-0678-6
Fares-Taie L, Gerber S, Chassaing N, et al. ALDH1A3 mutations cause recessive Anophthalmia and Microphthalmia. Am J Hum Genet. 2013;92(2):265–270. https://doi.org/10.1016/j.ajhg.2012.12.003
Pasutto F, Sticht H, Hammersen G, et al. Mutations in STRA6 cause a broad spectrum of malformations including Anophthalmia, congenital heart defects, diaphragmatic hernia, alveolar capillary dysplasia, lung hypoplasia, and mental retardation. Am J Hum Genet. 2007;80(3):550–560. https://doi.org/10.1086/512203
Plaisancié J, Ragge N, Dollfus H, et al. FOXE3 mutations: genotype‐phenotype correlations. Clin Genet. 2018;93(4):837–845. https://doi.org/10.1111/cge.13177
Garcia-Montalvo IA, Pelcastre-Luna E, Nelson-Mora J, Buentello-Volante B, Miranda-Duarte A, Zenteno JC. Mutational screening of FOXE3, GDF3, ATOH7, and ALDH1A3 in congenital ocular malformations. possible contribution of the FOXE3 p.VAL201MET variant to the risk of severe eye malformations. Ophthalmic Genet. 2014;35(3):190–192. https://doi.org/10.3109/13816810.2014.903983
Islam L, Kelberman D, Williamson L, et al. Functional analysis of FOXE 3 mutations causing dominant and recessive ocular anterior segment disease. Hum Mutat. 2015;36(3):296–300. https://doi.org/10.1002/humu.22741
Reis LM, Tyler RC, Schneider A, et al. FOXE3 plays a significant role in autosomal recessive microphthalmia. Am J Med Genet Part A. 2010;152A(3):582–590. https://doi.org/10.1002/ajmg.a.33257
Vidya NG, Rajkumar S, Vasavada AR. Genetic investigation of ocular developmental genes in 52 patients with anophthalmia/microphthalmia. Ophthalmic Genet. 2018;39(3):344–352. https://doi.org/10.1080/13816810.2018.1436184
Mory A, Ruiz FX, Dagan E, et al. A missense mutation in ALDH1A3 causes isolated microphthalmia/anophthalmia in nine individuals from an inbred Muslim kindred. Eur J Hum Genet. 2014;22:419–422. https://doi.org/10.1038/ejhg.2013.157
Roos L, Fang M, Dali C, et al. A homozygous mutation in a consanguineous family consolidates the role of ALDH1A3 in autosomal recessive microphthalmia. Clin Genet. 2014;86(3):276–281. https://doi.org/10.1111/cge.12277
Yahyavi M, Abouzeid H, Gawdat G, et al. ALDH1A3 loss of function causes bilateral anophthalmia/microphthalmia and hypoplasia of the optic nerve and optic chiasm. Hum Mol Genet. 2013;22(16):3250–3258. https://doi.org/10.1093/hmg/ddt179
Aldahmesh M, Khan A, Hijazi H, Alkuraya F. Mutations in ALDH1A3 cause microphthalmia. Clin Genet. 2013;84(2):128–131. https://doi.org/10.1111/cge.12184
Alabdullatif M, Al Dhaibani MA, Khassawneh MY, El‐Hattab AW. Chromosomal microarray in a highly consanguineous population: diagnostic yield, utility of regions of homozygosity, and novel mutations. Clin Genet. 2017;91(4):616–622. https://doi.org/10.1111/cge.12872
Boro A, Keita F, Sidibe FT, et al. Ocular manifestations in severe acute malnutrition in children under 60 months in a secondary health center. Open J Ophthalmol. 2023;13(3):288–294. https://doi.org/10.4236/ojoph.2023.133028
Dantas AP, Brandt CT, Leal DN. Ocular manifestations in patients who had malnutrition in the first six months of life. Arq Bras Oftalmol. 2005;68(6):753–756. https://doi.org/10.1590/S0004-27492005000600009
Verma AS, Fitzpatrick DR. Anophthalmia and microphthalmia. Orphanet J Rare Dis. 2007;2:e47. https://doi.org/10.1186/1750-1172-2-47
Cerrizuela S, Vega‐Lopez GA, Aybar MJ. The role of teratogens in neural crest development. Birth Defects Res. 2020;112(8):584–632. https://doi.org/10.1002/bdr2.1644
Dubucs C, Plaisancié J, Courtade-Saidi M, Damase-Michel C. The first review on prenatal drug exposure and ocular malformation occurrence. Front Pediat. 2024;12:e1379875. https://doi.org/10.3389/fped.2024.1379875
Howard R, Chataway J, Edwards M, et al. Toxic, metabolic and physical insults to the nervous system and inherited disorders of metabolism. In: Clarke C, Howard R, Rossor M, Shorvon S, eds. Neurology: A Queen Square Textbook. Wiley Publishers; 2016:729–796. https://doi.org/10.1002/9781118486160.ch19
Copyright (c) 2025 Usman Hameed, Ammara Saleem, Memoona Idrees, Muhammad Ansar

This work is licensed under a Creative Commons Attribution 4.0 International License.
Author(s) retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution (CC-BY) 4.0 License that allows others to share the work with an acknowledgment of the work’s authorship and initial publication in this journal.






