Association of Proprotein Convertase Subtilisin/Kexin Type 9 (PCSK9) Polymorphism with Atherosclerosis: A Bibliometric Analysis
Abstract
 Abstract Views: 0
Abstract Views: 0
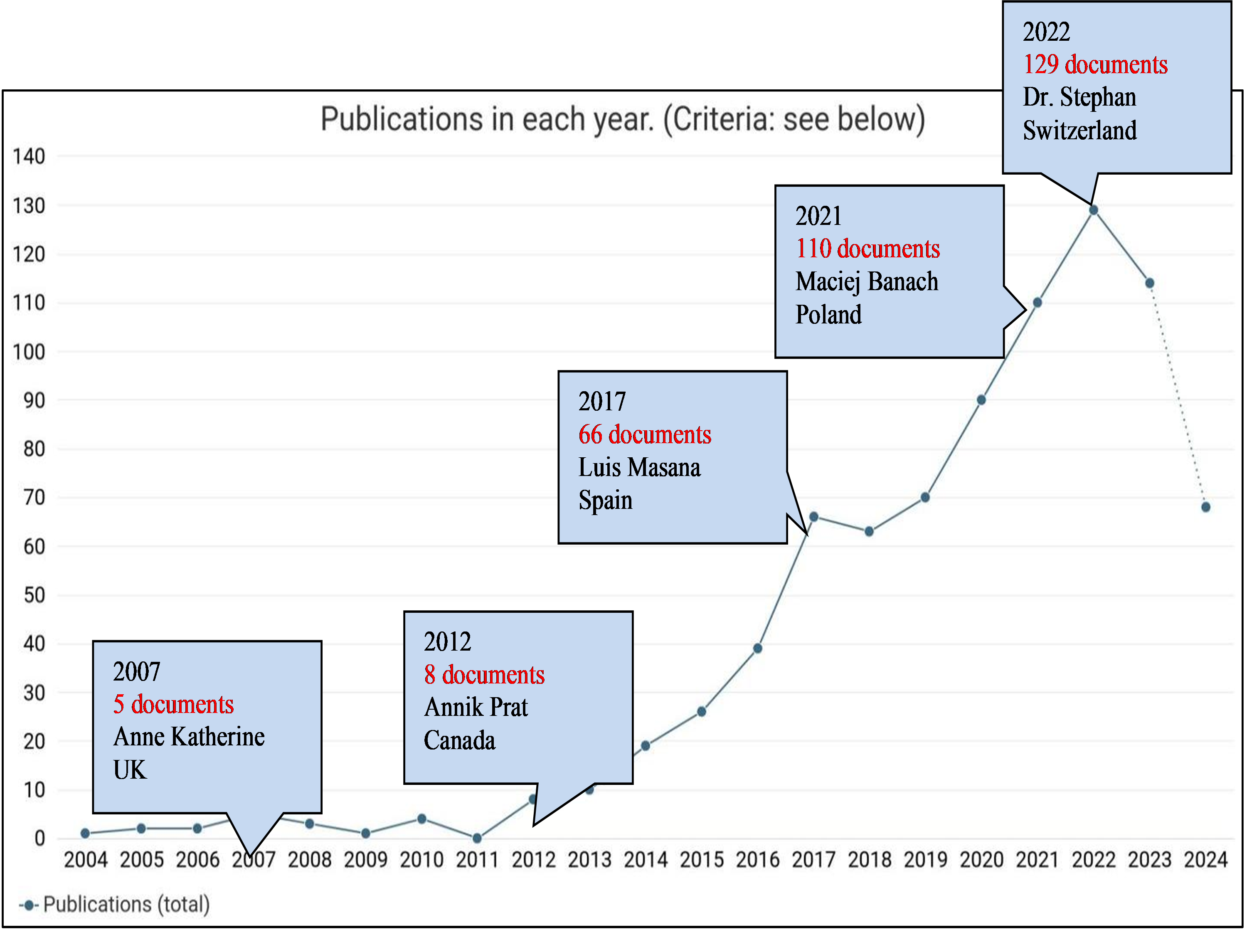
Bibliometric analysis offers a sophisticated approach to mapping the development and boundaries of a discipline. This study aimed to map global research trends on Proprotein Convertase Subtilisin or Kexin Type 9 (PCSK9) polymorphisms in atherosclerosis, an area with little previous investigation, using bibliometric analysis. PCSK9 is involved in the metabolism of cholesterol, impacting the risk of atherosclerotic cardiovascular disease (ASCVD). Understanding the relationship between PCSK9 polymorphisms and atherosclerosis mayhelp design suitable therapeutic strategies. Dimensions database was searched to retrieve research and review articles using query [TS = ((PCSK9 AND Polymorphism OR Variant) AND (Atherosclerosis))]. Articles published between 2004 and 2024 were included. VOS viewer software was used for data visualization and analysis. Total 816 research and review articles were retrieved. Research trend indicated a gradual rise in count of articles annually. Brigham and Women's Hospital, USA contributed the most in this research field. Robert Patrick Giugliano (Brigham and Women's Hospital, USA) and Marc Steven Sabatine (Brigham and Women's Hospital, USA) were the top contributors. In the discipline of atherosclerosis and cardiovascular diseases (CVDs), the high impacting journal is The European Heart Journal. Current research hot spots, such as hypercholesterolemia, PCSK9, atherosclerosis, statin therapy, and inflammation, were identified by a keyword analysis and major literature review. Recently, extensive interest in association of PCSK9 polymorphism with atherosclerosishas been explored internationally. Currently, the discipline is experiencing an upsurge in research with a focus on inflammation and coronary arteries.
Downloads
References
Townsend N, Kazakiewicz D, Lucy Wright F, et al. Epidemiology of cardiovascular disease in Europe. Nat Rev Cardiol. 2022;19:133-143. https://doi.org/10.1038/s41569-021-00607-3
Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35(42):2950-2959. https://doi.org/10.1093/eurheartj/ehu299
Trogdon JG, Finkelstein EA, Nwaise IA, Tangka FK, Orenstein D. The economic burden of chronic cardiovascular disease for major insurers. Health Promot Pract. 2007;8(3):234-242. https://doi.org/10.1177/1524839907303794
Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829-1830. https://doi.org/10.1001/jama.2021.5469
Blagov AV, Churov AV, Golovyuk AL, et al. The role of metabolic disorders in the development of atherosclerosis. Cell Mol Biol. 2024;70(9):148-155. https://doi.org/10.14715/cmb/2024.70.9.21
Barquera S, Pedroza-Tobías A, Medina C, et al. Global overview of the epidemiology of atherosclerotic cardiovascular disease. Arch Med Res. 2015;46(5):328-338. https://doi.org/10.1016/j.arcmed.2015.06.006
Ruparelia N, Chai JT, Fisher EA, Choudhury RP. Inflammatory processes in cardiovascular disease: a route to targeted therapies. Nat Rev Cardiol. 2017;14:133-144. https://doi.org/10.1038/nrcardio.2016.185
Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317-325. https://doi.org/10.1038/nature10146
Björkegren JL, Lusis AJ. Atherosclerosis: recent developments. Cell. 2022;185(10):1630-1645. https://doi.org/10.1016/j.cell.2022.04.004
Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937-952. https://doi.org/10.1016/S0140-6736(04)17018-9
Fernández-Friera L, Fuster V, López-Melgar B, et al. Normal LDL-cholesterol levels are associated with subclinical atherosclerosis in the absence of risk factors. J Am Coll Cardiol. 2017;70(24):2979-2991. https://doi.org/10.1016/j.jacc.2017.10.024
Nordestgaard BG, Chapman MJ, Humphries SE, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: Guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013;34(45):3478-3490. https://doi.org/10.1093/eurheartj/eht273
Schulz R, Schlüter K-D. PCSK9 targets important for lipid metabolism. Clin Res Cardiol Suppl. 2017;12:2-11. https://doi.org/10.1007/s11789-017-0085-0
Yurtseven E, Ural D, Baysal K, Tokgözoğlu L. An update on the role of PCSK9 in atherosclerosis. J Atheroscler Thromb. 2020;27(9):909-918. https://doi.org/10.5551/jat.55400
Seidah NG, Abifadel M, Prost S, Boileau C, Prat A, Touyz RM. The proprotein convertases in hypercholesterolemia and cardiovascular diseases: emphasis on proprotein convertase subtilisin/kexin 9. Pharmacol Rev. 2017;69(1):33-52. https://doi.org/10.1124/pr.116.012989
Seidah NG. The proprotein convertases, 20 years later. In: Mbikay M, Seidah NG. ed, Proprotein Convertases. 2011:23-57. https://doi.org/10.1007/978-1-61779-204-5_3
Schulz R, Schlüter K-D, Laufs U. Molecular and cellular function of the proprotein convertase subtilisin/kexin type 9 (PCSK9). Basic Res Cardiol. 2015;110:e4. https://doi.org/10.1007/s00395-015-0463-z
Ferri N, Tibolla G, Pirillo A, et al. Proprotein convertase subtilisin kexin type 9 (PCSK9) secreted by cultured smooth muscle cells reduces macrophages LDLR levels. Atherosclerosis. 2012;220(2):381-386. https://doi.org/10.1016/j.atherosclerosis.2011.11.026
Hampton EN, Knuth MW, Li J, Harris JL, Lesley SA, Spraggon G. The self-inhibited structure of full-length PCSK9 at 1.9 Å reveals structural homology with resistin within the C-terminal domain. Proc Natl Acad Sci. 2007;104(37):14604-14609. https://doi.org/10.1073/pnas.0703402104
Benjannet S, Rhainds D, Essalmani R, et al. NARC-1/PCSK9 and its natural mutants: zymogen cleavage and effects on the low density lipoprotein (LDL) receptor and LDL cholesterol. J Biol Chem. 2004;279(47):48865-48875. https://doi.org/10.1074/jbc.M409699200
Seidah NG, Benjannet S, Wickham L, et al. The secretory proprotein convertase neural apoptosis-regulated convertase 1 (NARC-1): Liver regeneration and neuronal differentiation. Proc Natl Acad Sci. 2003;100(3):928-933. https://doi.org/10.1073/pnas.0335507100
Kwon HJ, Lagace TA, McNutt MC, Horton JD, Deisenhofer J. Molecular basis for LDL receptor recognition by PCSK9. Proc Natl Acad Sci. 2008;105(6):1820-1825. https://doi.org/10.1073/pnas.0712064105
Shapiro MD, Tavori H, Fazio S. PCSK9: from basic science discoveries to clinical trials. Circ Res. 2018;122(10):1420-1438. https://doi.org/10.1161/CIRCRESAHA.118.311227
Matías-Pérez D, Pérez-Santiago A, Medina MS, Osorno JA, García-Montalvo I. PCSK9 gene participates in the development of primary dyslipidemias. Balkan J Med Genet. 2021;24(1):5-14. https://doi.org/10.2478/bjmg-2021-0009
Hopkins PN, Defesche J, Fouchier SW, et al. Characterization of autosomal dominant hypercholesterolemia caused by PCSK9 gain of function mutations and its specific treatment with alirocumab, a PCSK9 monoclonal antibody. Circ Cardiovasc Genet. 2015;8(6):823-831. https://doi.org/10.1161/CIRCGENETICS.115.001129
Sun H, Samarghandi A, Zhang N, Yao Z, Xiong M, Teng BB. Proprotein convertase subtilisin/kexin type 9 interacts with apolipoprotein B and prevents its intracellular degradation, irrespective of the low-density lipoprotein receptor. Arterioscler Thromb Vasc Biol. 2012;32(7):1585-1595. https://doi.org/10.1161/ATVBAHA.112.250043
He X-M, Chen L, Wang T-S, Zhang Y-B, Luo J-B, Feng X-X. E670G polymorphism of PCSK9 gene of patients with coronary heart disease among Han population in Hainan and three provinces in the northeast of China. Asian Pac J Trop Med. 2016;9(2):172-176. https://doi.org/10.1016/j.apjtm.2016.01.008
Cariou B, Ouguerram K, Zaïr Y, et al. PCSK9 dominant negative mutant results in increased LDL catabolic rate and familial hypobetalipoproteinemia. Arterioscler Thromb Vasc Biol. 2009;29(12):2191-2197. https://doi.org/10.1161/ATVBAHA.109.194191
Zheng M, Fu H-Z, Ho Y-S. Research trends and hotspots related to ammonia oxidation based on bibliometric analysis. Environ Sci Pollut Res. 2017;24:20409-20421. https://doi.org/10.1007/s11356-017-9711-0
Chen C, Song M. Visualizing a field of research: a methodology of systematic scientometric reviews. PloS One. 2019;14(10):e0223994. https://doi.org/10.1371/journal.pone.0223994
Van Eck N, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523-538. https://doi.org/10.1007/s11192-009-0146-3
Tang M, Yang S, Zou J, et al. Global trends and research hotspots of PCSK9 and cardiovascular disease: A bibliometric and visual analysis. Front Cardiovasc Med. 2024;11:e1336264. https://doi.org/10.3389/fcvm.2024.1336264
Wang Y, Lu X, Yue X, Kan L, Du S. Bibliometric analysis of PCSK9 inhibitors for cardiovascular disease management based on Web of Science. J Chin Pharm Sci. 2025;34(3):232. https://doi.org/10.5246/jcps.2025.03.018
Cui J, Zhang Y, Zhang W, et al. Research hotspots and development trends on apolipoprotein B in the field of atherosclerosis: a bibliometric analysis. Mol Biotechnol. 2025;67:2204-2222. https://doi.org/10.1007/s12033-024-01218-2
Tian W, Zhang T, Wang X, Zhang J, Ju J, Xu H. Global research trends in atherosclerosis: a bibliometric and visualized study. Front Cardiovasc Med. 2022;9:e956482. https://doi.org/10.3389/fcvm.2022.956482
Yang H, Zhang T, Wang D, et al. A systematic bibliometric analysis of cardiovascular disease risk in obesity (2014–2024). J Multidiscip Healthc. 2025;18:3233–3255. https://doi.org/10.2147/JMDH.S504022
Jia B, Wei R, Yuan C, et al. A bibliometric analysis of vaccination against atherosclerosis. Hum Vaccines Immunother. 2024;20(1):e2365500. https://doi.org/10.1080/21645515.2024.2365500
Lai P, Xu S, Liu Z, et al. Exploring research trends and hotspots on PCSK9 inhibitor studies: A bibliometric and visual analysis spanning 2007 to 2023. Front Cardiovasc Med. 2024;11:e1474472. https://doi.org/10.3389/fcvm.2024.1474472
Cheng Q, Sun J, Zhong H, et al. Research trends in lipid-lowering therapies for coronary heart disease combined with hyperlipidemia: a bibliometric study and visual analysis. Front Pharmacol. 2024;15:e1393333. https://doi.org/10.3389/fphar.2024.1393333
Ragusa R, Rocchiccioli S, Del Turco S, et al. PCSK9 and coronary atherosclerosis progression beyond LDL-cholesterol in coronary artery disease patients. Eur J Clin Invest. 2025;e70083. https://doi.org/10.1111/eci.70083
Ma J, Zhao K, Zhu Y, Xu W, Huang J, Wei X, et al. Bibliometric analysis of monoclonal antibodies for atherosclerosis. Hum Vaccines Immunother. 2023;19(3):e2266926. https://doi.org/10.1080/21645515.2023.2266926
Copyright (c) 2025 Rafia, Sehrish Basheer, Adila Khalil, Misbah Hussain

This work is licensed under a Creative Commons Attribution 4.0 International License.
Author(s) retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution (CC-BY) 4.0 License that allows others to share the work with an acknowledgment of the work’s authorship and initial publication in this journal.






