Molecular Characterization of Rifampicin Associated Mutation in Mycobacterium tuberculosis Isolates
Abstract
 Abstract Views: 224
Abstract Views: 224
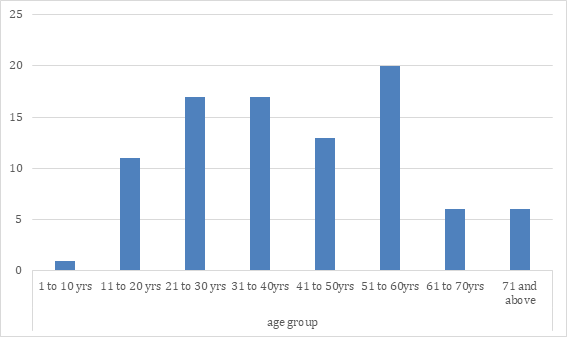
Mycobacterium tuberculosis is one of the most lethal pathogens causing infection in 1.8 billion people annually. M. tuberculosis majorly cause pulmonary infection which spreads easily by the air. Rifampicin is a first line drug used for the treatment of this disease. By binding to the 30S ribosomal subunit it inhibits the protein synthesis. The misuse of this drug and incomplete treatment causes alteration at the genetic level of rpoB gene of the MTB. The aim of our study was to find the mutations in the rpoB gene from the clinical isolates of the tuberculosis patients. We collected 412 sputum samples from patients suspected of tuberculosis and cultured in the microbiology laboratory of THQ Fatehpur, Layyah. Positive sputum cultures were analyzed for drug susceptibility test. Genomic DNA was isolated by sonication method using 20 Hz frequency of ultrasonic waves. After that primers were designed using bioinformatics tools for amplification of the gene. Additionally, the rpoB was amplified by a hemi-nested PCR technique. 91 samples were positive for sputum culture which consisted of 54 males and 37 females. Out of the 91 positive cultures, four samples showed rifampicin resistance. Two samples carried single missense mutation at position 526 and 531 in the amino acid sequence of rpoB gene whereas third and fourth sample carried a single missense mutation at position 516 in the amino acid sequence of rpoB gene. Moreover, 22% of the tested sputum samples were positive for tuberculosis. This means that in the population of tehsil Fatehpur, Layyah tuberculosis is prevalent. Furthermore, 4.3% of this 22% were found to be rifampicin resistant. In the future researches the harmful effect of rpoB gene mutations which is associated with function of the β-subunit of RNA polymerase in 16S rRNA and its interaction with rifampicin can be estimated by performing molecular docking
Copyright (c) 2021 Ali Tahir, Rumesha Rafiq, Shahzeb Khan, Zaman Khan, Imran Tipu
Downloads
References
Todar K. Online textbook of bacteriology. University of Wisconsin-Madison Department of Bacteriology. 2008.
Narayan P, PGIMS CI. Tuberculosis: The Causes, Prevention and Diagnosis. Int J Pharma Bio Sci Fundamentals. 2012;1(1):1-3.
Todar K. Mycobacterium tuberculosis and Tuberculosis. Online text book of bacteriology Madison, Wisconsin. 2008.
Cegielski JP, McMurray DN. The relationship between malnutrition and tuberculosis: Evidence from studies in humans and experimental animals. Int J Tubercu Lung Dis. 2004;8(3):286-98.
Imtiaz S, Shield KD, Roerecke M, Samokhvalov AV, Lönnroth K, Rehm J. Alcohol consumption as a risk factor for tuberculosis: Meta-analyses and burden of disease. Eur Respir J. 2017;50(1):1-13.
Blumberg HM, Leonard MK, Jasmer RM. Update on the treatment of tuberculosis and latent tuberculosis infection. Jama. 2005;293(22):2776-2784.
Van Soolingen DI, Hermans PW, De Haas PE, Soll DR, Van Embden JD. Occurrence and stability of insertion sequences in Mycobacterium tuberculosis complex strains: Evaluation of an insertion sequence-dependent DNA polymorphism as a tool in the epidemiology of tuberculosis. J Clin Microbiol. 1991;29(11):2578-86. https://doi.org/10.1128/jcm.29.11.2578-2586.1991
Chang KC, Yew WW. Management of difficult multidrug‐resistant tuberculosis and extensively drug‐resistant tuberculosis: update 2012. Respir. 2013;18(1):8-21. https://doi.org/10.1111/j.1440-1843.2012.02257.x
Chiang CY, Centis R, Migliori GB. Drug‐resistant tuberculosis: Past, present, future. Respir. 2010;15(3):413-432. https://doi.org/10.1111/j.1440-1843.2010.01738.x
Kim DH, Kim HJ, Park S-K, et al. Treatment outcomes and survival based on drug resistance patterns in multidrug-resistant tuberculosis. Ame J Respir Critical Care Med. 2010;182(1):113-119. https://doi.org/10.1164/rccm.200911-1656OC
Migliori G, Lange C, Girardi E, et al. Fluoroquinolones: are they essential to treat multidrug-resistant tuberculosis? Eur Respir J. 2008;31(4):904-905.
Organization WH. Global tuberculosis report 2013. World Health Organization; 2013.
Bastos ML, Hussain H, Weyer K, et al. Treatment outcomes of patients with multidrug-resistant and extensively drug-resistant tuberculosis according to drug susceptibility testing to first-and second-line drugs: an individual patient data meta-analysis. Clin Infect Dis. 2014;59(10):1364-1374.
Rie AV, Page-Shipp L, Scott L, Sanne I, Stevens W. Xpert® MTB/RIF for point-of-care diagnosis of TB in high-HIV burden, resource-limited countries: hype or hope? Expert Rev Mol Diagn. 2010;10(7):937-946. https://doi.org/10.1586/erm.10.67
Yam W, Tam C, Leung C, et al. Direct detection of rifampin-resistant Mycobacterium tuberculosis in respiratory specimens by PCR-DNA sequencing. J Clin Microbiol. 2004;42(10):4438-4443. https://doi.org/10.1128/JCM.42.10.4438-4443.2004
Sinha P, Srivastava G, Tripathi R, Mishra MN, Anupurba S. Detection of mutations in the rpoB gene of rifampicin-resistant Mycobacterium tuberculosis strains inhibiting wild type probe hybridization in the MTBDR plus assay by DNA sequencing directly from clinical specimens. BMC Microbiol. 2020;20(1):1-8. https://doi.org/10.1186/s12866-020-01967-5
Organization WH. Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB. World Health Organization; 2013. 9241506334.
Organization WH. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. World Health Organization; 2014.
Mokrousov I, Otten T, Vyshnevskiy B, Narvskaya O. Allele-specific rpoB PCR assays for detection of rifampin-resistant Mycobacterium tuberculosis in sputum smears. Antimicrobial Agents and Chemotherapy. 2003;47(7):2231-2235. https://doi.org/10.1128/AAC.47.7.2231-2235.2003
Rasool G, Khan AM, Mohy-Ud-Din R, Riaz M. Detection of Mycobacterium tuberculosis in AFB smear-negative sputum specimens through MTB culture and GeneXpert® MTB/RIF assay. Int J Immunopathol Pharma. 2019;33:1-6. https://doi.org/10.1177/2058738419827174
Palaci M, Ueki SY, Sato DN, Telles MD, Curcio ME, Silva EA. Evaluation of mycobacteria growth indicator tube for recovery and drug susceptibility testing of Mycobacterium tuberculosis isolates from respiratory specimens. J Clin Microbiol. 1996;34(3):762-764. https://doi.org/10.1128/jcm.34.3.762-764.1996
Klein D. Quantification using real-time PCR technology: applications and limitations. Trends Mol Med. 2002;8(6):257-260. https://doi.org/10.1016/S1471-4914(02)02355-9
Caviedes L, Lee TS, Gilman RH, et al. Rapid, efficient detection and drug susceptibility testing of Mycobacterium tuberculosis in sputum by microscopic observation of broth cultures. The Tuberculosis Working Group in Peru. J Clin Microbiol. 2000;38(3):1203-1208. https://doi.org/10.1128/JCM.38.3.1203-1208.2000
Mboowa G, Namaganda C, Ssengooba W. Rifampicin resistance mutations in the 81 bp RRDR of rpoB gene in Mycobacterium tuberculosis clinical isolates using Xpert® MTB/RIF in Kampala, Uganda: a retrospective study. BMC Infect Dis. 2014;14(1):1-5. https://doi.org/10.1186/1471-2334-14-481
Ullah I, Javaid A, Tahir Z, et al. Pattern of drug resistance and risk factors associated with development of drug resistant Mycobacterium tuberculosis in Pakistan. Plos One. 2016;11(1):e0147529. https://doi.org/10.1371/journal.pone.0147529
Ramaswamy S, Musser JM. Molecular genetic basis of antimicrobial agent resistance inMycobacterium tuberculosis: 1998 update. Tuber Lung Dis. 1998;79(1):3-29. https://doi.org/10.1054/tuld.1998.0002
Rasool G, Khan AM, Mohy-Ud-Din R, Riaz M. Detection of Mycobacterium tuberculosis in AFB smear-negative sputum specimens through MTB culture and GeneXpert® MTB/RIF assay. Int J Immunopathol Pharmacol. 2019;33:3-29. https://doi.org/10.1177/2058738419827174
Schön T, Miotto P, Köser CU, Viveiros M, Böttger E, Cambau E. Mycobacterium tuberculosis drug-resistance testing: challenges, recent developments and perspectives. Clin Microbiol Infect. 2017;23(3):154-160. https://doi.org/10.1016/j.cmi.2016.10.022
Bainomugisa A, Wampande E, Muchwa C, et al. Use of real time polymerase chain reaction for detection of M. tuberculosis, M. avium and M. kansasii from clinical specimens. BMC Infect Dis. 2015;15(1):1-7. https://doi.org/10.1186/s12879-015-0921-0
Negi S, Khan SF, Gupta S, Pasha S, Khare S, Lal S. Comparison of the conventional diagnostic modalities, bactec culture and polymerase chain reaction test for diagnosis of tuberculosis. Indian J Med Microbiol. 2005;23(1):29-33. https://doi.org/10.1016/S0255-0857(21)02708-0
Hameed S, Moganeradj K, Mahmood N, et al. Sequence analysis of the rifampicin resistance determining region (RRDR) of rpoB gene in multidrug resistance confirmed and newly diagnosed tuberculosis patients of Punjab, Pakistan. PloS one. 2017;12(8):e0183363. https://doi.org/10.1371/journal.pone.0183363
Copyright (c) 2021 Ali Tahir, Rumesha Rafiq, Shahzeb Khan , Zaman Khan, Imran Tipu

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










