Monocyte-to-Lymphocyte Ratio (MLR) as a Possible Prognostic Marker of Latent Tuberculosis (LTBI) among Household Contacts of Active Tuberculosis (TB) Patients
Abstract
 Abstract Views: 288
Abstract Views: 288
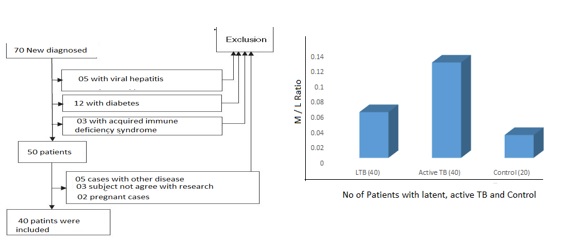
Tuberculosis (TB) is endemic in many low socio-economic/developing countries including Pakistan. It is a leading cause of death from a single infectious agent worldwide. Identification and early treatment of latent conditions help reduce the complications associated with TB. However, the identification of individuals with latent infection is a time taking and expensive process. According to previous studies, a promising and cheap biomarker of TB may be the monocyte-to-lymphocyte ratio (MLR). It may indicate a body’s immune response to Mycobacterium tuberculosis. Since household contacts of tuberculosis (TB) patients have an increased risk of latent tuberculosis (LTBI), using the established diagnostic procedures as well as checking their MLR might help determine if they contracted LTBI or not. We conducted a cross-sectional study to determine if MLR could be used to identify LTBI among household contacts of patients with active tuberculosis. Out of the 100 subjects selected for this study, about 40 patients were recently diagnosed with active tuberculosis, 40 were close contacts of these patients, while 20 were chosen to be controls. The mean MLRwas 0.165, 0.06 (range 0.03–0.08), and 0.04 (0.02–0.04) in patients with active tuberculosis, close contacts of patients, and control subjects, respectively. Hence, it was determined that MLR (> 06 %) is a significant predictor for LTBI and can be used to diagnose it in close contacts of TB patients. It was additionally observed that patients over the age of 50 with pulmonary tuberculosis have higher MLR. Ratio of monocytes to lymphocytes (> 0.06) may help in diagnosing latent tuberculosis in close contacts of tuberculosis patients.
Downloads
References
Zaidi SM, Waseem HF, Ansari FA, Irfan M, Fahim S, Ahmad M. Sample size estimation of diagnostic test
studies in health sciences. In14th Int Conference on 2016 (p. 239).
Al Hajoj S, Varghese B, Datijan A, et al. Interferon gamma release assay versus tuberculin skin testing among healthcare workers of highly diverse origin in a moderate tuberculosis burden country. PloSOne. 2016;11(5):0154803.https://doi.org/10.1371/journal.pone.0154803
Sadaf R, Munir T, Farrukh S, Abbasi S. Prevalence of latent tuberculosis infection in healthcare workers in tertiary care hospitals of Pakistan. Pak J Med Sci. 2020;36(2):198-202. https://doi.org/10.12669/pjms.36.2.936
Wang J, Yin Y, Wang X, et al. Ratio of monocytes to lymphocytes in peripheral blood in patients diagnosed with active tuberculosis. Braz J Infect Dis 2015;19(2):125-31.https://doi.org/10.1016/j.bjid.2014.10.008
Sibley L, Gooch K, Wareham A, et al. Differences in monocyte: lymphocyte ratio and Tuberculosis disease progression in genetically distinct populations of macaques. Sci Rep. 2019;9(1):1-9.
Yang J, Zhang L, Yu C, Yang XF, Wang H. Monocyte and macrophage differentiation: circulation inflammatory monocyte as biomarker for inflammatory diseases. Biomark Res. 2014;7(2):1-2. https://doi.org/10.1186/2050-7771-2-1
Esmail H, Barry III CE, Wilkinson RJ. Understanding latent tuberculosis: The key to improved diagnostic and novel treatment strategies. Discov Today. 2012;17(9-10):51421.https://doi.org/10.1016/j.drudis.2011.12.013
Ahmad S. Pathogenesis, Immunology, and Diagnosis of Latent Mycobacterium Tuberculosis Infection. Clin& Develop Immunol. 2010;2011:1–2.
Mayito J, Meya DB, Rhein J, Sekaggya-Wiltshire C. Utility of the monocyte to lymphocyte ratio in diagnosing latent tuberculosis among HIV-infected individuals with a negative tuberculosis symptom screen. PLoS One. 2020;15(11):e0241786.https://doi.org/10.1371/journal.pone.0241786
Yang J, Lee S, Oh S, et al. The risk of active tuberculosis among individuals living in tuberculosis-affected households in the Republic of Korea, 2015. PLoS ONE 2019; 14(12):e0225744. https://doi.org/10.1371
Simon D, Simon HU, Yousefi S. Extracellular DNA traps in allergic, infectious, and autoimmune diseases. Allergy. 2013;68(4):409–16.
Marahatta SB, Yadav RK, Giri D, et al. Barriers in the access, diagnosis and treatment completion for tuberculosis patients in central and western Nepal: A qualitative study among patients, community members and health care workers. PLoS ONE 2020;15(1):e0227293.https://doi.org/10.1371/journal.pone.0227293
Watkins RE, Plant AJ. Does smoking explain sex differences in the global tuberculosis epidemic? Epidemiol Infect. 2006;134:333–9.
Lee H, Kim J, Ae Kang Y, et al. In vitro Mycobacterial Growth Inhibition in South Korean Adults with Latent TB Infection.Front Immunol. 2019;10:896https://doi.org/10.3389/fi mmu.2019.00896
La Manna MP, Orlando V, Dieli F, et al. Quantitative and qualitative profiles of circulating monocytes may help identifying tuberculosis infection and disease stages. PLoS One. 2017;12(2):e0171358. https://doi.org/10.1371/journal.pone.0171358
Philips JA, Ernst JD. Tuberculosis pathogenesis and immunity, Annual Review of Pathology: Mech Dis. 2012;7(1):353–384
Wang W, Wang L, Liu YY, et al. Value of the Ratio of Monocytes to Lymphocytes for Monitoring Tuberculosis Therapy. Canadian J Infectious Dis Med Microbiol 2019;2019:1-5.
Naranbhai V, Fletcher HA, Tanner R, et al. Distinct transcriptional and antimycobacterial profiles of peripheral blood monocytes dependent on the ratio of monocytes: lymphocytes. EBioMed. 2015;2(11):1619-26. https://doi.org/10.1016/j.ebiom.2015.0 9.027
Liu C, Liu H, Ge B. Innate immunity in tuberculosis: host defense vs pathogen evasion. Cell MolImmunol 2017;14:963–975. https://doi.org/10.1038/cmi.2017.88
Rakotosamimanana N, Richard V, Raharimanga V, Gicquel B, Doherty M, Zumla A. Biomarkers for risk of 10
developing active tuberculosis in contacts of TB patients. Eur Respir J 2015;46(4):1095-103.
Liana P, Brestilova B, Rahadiyanto KY. The ratio of monocytes to lymphocytes accuracy as tuberculosis predictor. InJournal of Physics: Conference Series 2019 Jul 1 (Vol. 1246, No. 1, p. 012024). IOP Publishing.
De Martino M, lodi L, Galli L, Chiapinni E. Immune Response to Mycobacterium tuberculosis: A Narrative Review. FrontPediatr. 2019;7:1-8. https://doi.org/10.3389/ fped.2019.00350
Reece ST, Vogelzang A, Tornack J, et al. Mycobacterium TuberculosisInfected Hematopoietic Stem and Progenitor Cells Unable to Express Inducible Nitric Oxide Synthase Propagate Tuberculosis in Mice. J Infect Dis. 2018;217(10):1667-1671. https://doi.org/10.1093/infdis/jiy041
Iqbal S, Ahmad U, Zaidi SBH. Monocyte Lymphocyte Ratio as a Possible Prognostic Marker in Ant tuberculous Therapy. J Rawal Med College. 2014;18(2):178-181.
Tabassum MN, Muhammad AK, Afzal S, Gilani A, Gureja AW, Tabassum S. Demographic Characteristics of Tuberculosis Patients at Public Sector Health Facilities in Lahore, Pakistan. Ann of King Edward Med Univ. 2018;24:16.https://doi.org/10.21649/akemu.v24i1.2309
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.