Polycystic Ovary Syndrome (PCOS): A Concerning Hormonal Condition and its Bodily Impact on Women
Abstract
 Abstract Views: 167
Abstract Views: 167
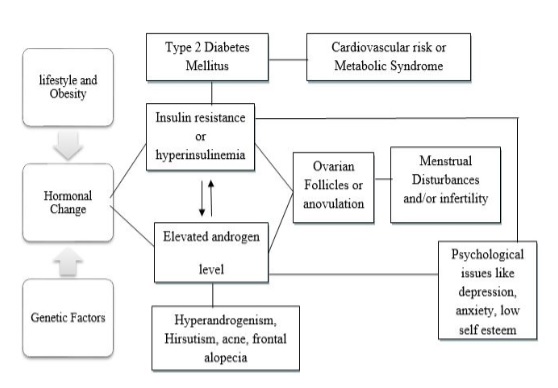
Polycystic Ovary Syndrome (PCOS) is a prevalent hormonal disorder that have severe health consequences for women. It arises in the early puberty stage and affects a large percentage of the world’s population. While the exact cause is unknown, it’s known to cause hyperandrogenism, insulin resistance, menstrual irregularities, and ovulatory dysfunction, all of which can lead to infertility and endometrial cancer. Long-term cardiometabolic risks and comorbidities are seen in both slim and obese PCOS patients. Given these serious implications, it’s
critical to fully comprehend the pathophysiological relationships that underpin PCOS, so that better treatment plans can be developed and the standard of living for women having this condition may improve. This condition is diagnosed using three separate criteria. Rotterdam criterion is mostly utilized for PCOS diagnosis. Different symptoms of PCOS are treated in different ways. It’s imperative to comprehensively treat these patients as soon as possible in order to cope with the emotion burden associated with the disease that is often ignored. PCOS
can be managed by early diagnosis and long-term treatment, allowing women to maintain a healthy lifestyle and avoiding long-term complications, including metabolic syndrome and cardiovascular diseases.
Downloads
References
Witchel SF, Oberfield SE, Peña AS. Polycystic ovary syndrome: Pathophysiology, presentation, and treatment with emphasis on adolescent girls. J Endocr Soc. 2019;3(8):1545-1573. https://doi.org/10.1210/js.2019-00078
El Hayek S, Bitar L, Hamdar LH, Mirza FG, Daoud G. Poly cystic ovarian syndrome: An updated overview. Front Physiol. 2016;7:124. https://doi.org/10.3389/fphys.2016.00124
Ashraf S, Nabi M, Rashid F, Amin S. Hyperandrogenism in polycystic ovarian syndrome and role of CYP gene variants: A review. Egypt J Med Hum Genet. 2019;20(1):1-10. https://doi.org/10.1186/s43042-019-0031-4
Rosenfield RL, Ehrmann DA. The pathogenesis of polycystic ovary syndrome (PCOS): The hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr Rev. 2016;37(5):467-520. https://doi.org/10.1210/er.2015-1104
Tabassum F, Jyoti C, Sinha HH, Dhar K, Akhtar MS. Impact of polycystic ovary syndrome on quality of life of women in correlation to age, basal metabolic index, education and marriage. PloS One. 2021;16(3):e0247486. https://doi.org/10.1371/journal.pone.0247486
Sidra S, Tariq MH, Farrukh MJ, Mohsin M. Evaluation of clinical manifestations, health risks, and quality of life among women with polycystic ovary syndrome. PLoS One. 2019;14(10):e0223329. https://doi.org/10.1371/journal.pone.0223329
Hajivandi L, Noroozi M, Mostafavi F, Ekramzadeh M. Food habits in overweight and obese adolescent girls with Polycystic ovary syndrome (PCOS): A qualitative study in Iran. BMC Pediatr. 2020;20(1):277. https://doi.org/10.1186/s12887-020-02173-y
Spritzer PM, Barone CR, Oliveira FB. Hirsutism in polycystic ovary syndrome: Pathophysiology and management. Curr Pharm Des. 2016;22(36):5603-5613. https://doi.org/10.2174/1381612822666160720151243
Ding T, Hardiman PJ, Petersen I, Wang FF, Qu F, Baio G. The prevalence of polycystic ovary syndrome in reproductive-aged women of different ethnicity: A systematic review and meta-analysis. Oncotarget. 2017;8(56):96351-96358. https://doi.org/10.18632/oncotarget.19180
Papadakis G, Kandaraki EA, Tseniklidi E, Papalou O, Diamanti-Kandarakis E. Polycystic ovary syndrome and NC-CAH: distinct characteristics and common findings. A systematic review. Front Endocrinol. 2019;19;10:e388. https://doi.org/10.3389/fendo.2019.00388
Orbetzova MM. Clinical Impact of Insulin Resistance in Women with Polycystic Ovary Syndrome. In: Wang Z, ed. Polycystic ovarian syndrome. Intech Open; 2020. https://doi.org/10.5772/intechopen.90749
Calcaterra V, Verduci E, Cena H, et al. Polycystic ovary syndrome in insulin-resistant adolescents with obesity: The role of nutrition therapy and food supplements as a strategy to protect fertility. Nutrients. 2021;13(6):e1848. https://doi.org/10.3390/nu13061848
Sanchez-Garrido MA, Tena-Sempere M. Metabolic dysfunction in polycystic ovary syndrome: Pathogenic role of androgen excess and potential therapeutic strategies. Mol Metab. 2020;35:e100937. https://doi.org/10.1016/j.molmet.2020.01.001
Joseph S, Barai RS, Bhujbalrao R, Idicula-Thomas S. PCOSKB: A knowledge base on genes, diseases, ontology terms and biochemical pathways associated with poly cystic ovary syndrome. Nucleic Acids Res. 2016;44(D1):D1032-D1035. https://doi.org/10.1093/nar/gkv1146
Ajmal N, Khan SZ, Shaikh R. Polycystic ovary syndrome (PCOS) and genetic predisposition: A review article. Eur J Obstet Gyneco Reprod Biol X. 2019;3:e100060. https://doi.org/10.1016/j.eurox.2019.100060
Chen Y, Fang SY. Potential genetic polymorphisms predicting polycystic ovary syndrome. Endocr Connect. 2018;7(5):R187-R195. https://doi.org/10.1530/EC-18-0121
De Leo V, Musacchio MC, Cappelli V, Massaro MG, Morgante G, Petraglia FJ. Genetic, hormonal and metabolic aspects of PCOS: An update. Reproduc Biol Endocrin. 2016;14(1):1-17. https://doi.org/10.1186/s12958-016-0173-x
Ding H, Zhang J, Zhang F, et al. Resistance to the insulin and elevated level of androgen: A major cause of polycystic ovary syndrome. Front Endocrinol. 2021;12:e741764. https://doi.org/10.3389/fendo.2021.741764
Chaudhary H, Patel J, Jain NK, Joshi R. The role of polymorphism in various potential genes on polycystic ovary syndrome susceptibility and pathogenesis. J Ovarian Res. 2021;14(1):e125. https://doi.org/10.1186/s13048-021-00879-w
Ali RJ. Genetic polymorphism in MTHFR and PCO genes associated with the incidence of polycystic ovary syndrome in a sample of Iraqi women [Master thesis]. Al-Nahrain University/ College of Science, Iraq; 2016.
Khan MJ, Ullah A, Basit S. Genetic basis of polycystic ovary syndrome (PCOS): Current perspectives. Appl Clin Genet. 2019;12:249-260. https://doi.org/10.2147/TACG.S200341
Wang F, Wang Z. Diagnosis, pathogenesis and management of polycystic ovary syndrome. In: Darwish AM, ed. Testes and ovaries-functional and clinical differences and similarities. Intech Open; 2017. https://doi.org/10.5772/67877
Havelock J. Poly cystic ovary syndrome. Br C Med J. 2018;60(4):210-216.
Jahan Z, Wing KE. Polycystic ovary syndrome and its relationship with infertility and its management. J Bangladesh Coll Phys Surg. 2021;39(1):53-58. https://doi.org/10.3329/jbcps.v39i1.50458
Helvaci N, Karabulut E, Demir AU, Yildiz BO. Polycystic ovary syndrome and the risk of obstructive sleep apnea: A meta-analysis and review of the literature. Endocr Connect. 2017;6(7):437-445. https://doi.org/10.1530/EC-17-0129
Unluhizarci K, Karaca Z, Kelestimur F. Role of insulin and insulin resistance in androgen excess disorders. World J Diabetes. 2021;12(5):616-629. https://doi.org/10.4239/wjd.v12.i5.616
Christodoulopoulou V, Trakakis E, Pergialiotis V, et al. Clinical and biochemical characteristics in PCOS women with menstrual abnormalities. J Family Reprod Health. 2016;10(4):184-190.
Harris HR, Titus LJ, Cramer DW, Terry KL. Long and irregular menstrual cycles, polycystic ovary syndrome, and ovarian cancer risk in a population-based case-control study. Int J Cancer. 2017;140(2):285-291. https://doi.org/10.1002/ijc.30441
Huang S, Pang Y, Yan J, et al. Fractalkine restores the decreased expression of StAR and progesterone in granulosa cells from patients with polycystic ovary syndrome. Sci Rep. 2016;6(1):1-9. https://doi.org/10.1038/srep26205
Mohammad MB, Seghinsara AM. Polycystic ovary syndrome (PCOS), diagnostic criteria, and AMH. Asian Pac J Cancer Prev. 2017;18(1):17-21. https://doi.org/10.22034/APJCP.2017.18.1.17
Sachdeva G, Gainder S, Suri V, Sachdeva N, Chopra S. Comparison of the different PCOS phenotypes based on clinical metabolic, and hormonal profile, and their response to clomiphene. Indian J Endocrinol Metab. 2019;23(3):326-331. https://doi.org/10.4103/ijem.IJEM_30_19
Williams T, Mortada R, Porter S. Diagnosis and treatment of polycystic ovary syndrome. Am Fam Physician. 2016;94(2):106-113.
Helvaci N, Yildiz BO. The impact of ageing and menopause in women with polycystic ovary syndrome. Clinic Endocrinol. 2022;97(3):371-82. https://doi.org/10.1111/cen.14558
McDonnell R, Hart RJ. Pregnancy-related outcomes for women with polycystic ovary syndrome. Women Health. 2017;13(3):89-97. https://doi.org/10.1177/1745505717731971
Wickham H. Poly cystic ovarian syndrome in India: A socio-cultural perspective. Independent Study Project Collection; 2018. https://digitalcollections.sit.edu/isp_collection/2993
Lolou V. The role of probiotics and symbiotic on hirsutism. Fermentation. 2021;7(1):e10. https://doi.org/10.3390/fermentation7010010
Joshi M, Shankar R, Pathak K, Yadav R. Polycystic ovarian syndrome: A review covering phytoconstituents for its outstrip management. Pharmacol Res-Mod Chinese Med. 2021;1:e100011.https://doi.org/10.1016/j.prmcm.2021.100011
Franik G, Bizoń A, Włoch S, Kowalczyk K, Biernacka-Bartnik A, Madej P. Hormonal and metabolic aspects of acne vulgaris in women with polycystic ovary syndrome. Eur Rev Med Pharmacol Sci. 2018;22(14):4411-4418. https://doi.org/10.26355/eurrev_201807_15491
Kutlubay Z, Kecici AS, Engin B, Serdaroglu S, Tuzun Y. Acne Vulgaris. In: Kartal SP, Gönül M, eds. Acne and acneiform eruptions. 2017:7-13. https://doi.org/10.5772/65639
Bulsara JP, Patel P, Soni A, Acharya S. A review on brief insight into polycystic ovarian syndrome. Endocrine Metabol Sci. 2021;3:e100085. https://doi.org/10.1016/j.endmts.2021.100085
Yau TT, Ng NY, Cheung LP, Ma RC. Polycystic ovary syndrome: A common reproductive syndrome with long-term metabolic consequences. Hong Kong Med J. 2017;23(6):622-634. https://doi.org/10.12809/hkmj176308
He Y, Zheng D, Shang W, et al. Prevalence of oligomenorrhea among women of childbearing age in China: A large community-based study. Women's Health. 2020;16. https://doi.org/10.1177/1745506520928617
Rebar R. Evaluation of amenorrhea, anovulation, and abnormal bleeding. In: DeGroot LJ, Chrousos G, Dungan K, et al., eds. Endotext. South Dartmouth, MA: MDText.com, Inc.; 2000
Newbery G, Neelakantan M, Cabral MD, Omar H. Amenorrhea in adolescents. Pediatr Med. 2019;2:e30. http://dx.doi.org/10.21037/pm.2019.06.06
De Leo V, Musacchio MC, Cappelli V, Massaro MG, Morgante G, Petraglia F. Genetic, hormonal and metabolic aspects of PCOS: An update. Reprod Biol Endocrinol. 2016;14(1):1-7. https://doi.org/10.1186/s12958-016-0173-x
Liu Q, Xie YJ, Qu LH, Zhang MX, Mo ZC. Dyslipidemia involvement in the development of polycystic ovary syndrome. Taiwanese J Obste Gynecol. 2019;58(4):447-53. https://doi.org/10.1016/j.tjog.2019.05.003
Osibogun O, Ogunmoroti O, Michos ED. Polycystic ovary syndrome and cardiometabolic risk: opportunities for cardiovascular disease prevention. Trends Cardiovascul Med. 2020;30(7):399-404. https://doi.org/10.1016/j.tcm.2019.08.010
Hosseinzadeh P, Barsky M, Gibbons WE, Blesson CS. Polycystic ovary syndrome and the forgotten uterus. F S Rev. 2021;2(1):11-20. https://doi.org/10.1016/j.xfnr.2020.12.001
Sulaiman MA, Al-Farsi YM, Al-Khaduri MM, Waly MI, Saleh J, Al-Adawi S. Psychological burden among women with polycystic ovarian syndrome in Oman: a case–control study. Int J Womens Health. 2017;9:897-904. https://doi.org/10.2147/IJWH.S145383
Louwers YV, Laven JSE. Characteristics of polycystic ovary syndrome throughout life. Ther Adv Reprod Health. 2020;14:e2633494120911038. https://doi.org/10.1177/2633494120911038
Koneru A. Polycystic ovary syndrome (PCOS) and sexual dysfunctions. J Psychosex Health. 2019;1(2):154-158. https://doi.org/10.1177/2631831819861471
Meun C, Gunning MN, Louwers YV, et al. The cardiovascular risk profile of middle‐aged women with polycystic ovary syndrome. Clinic Endocrinol. 2020;92(2):150-158. https://doi.org/10.1111/cen.14117
Ding DC, Chen W, Wang JH, Lin SZ. Association between polycystic ovarian syndrome and endometrial, ovarian, and breast cancer: A population-based cohort study in Taiwan. Medicine. 2018;97(39):e12608. https://doi.org/10.1097/MD.0000000000012608
McCartney CR, Marshall JC. Clinical practice. Polycystic Ovary Syndrome. N Engl J Med. 2016;375(1):54-64. https://doi.org/10.1056/NEJMcp1514916
Chen H, Zhang Y, Li S, et al. The genetic association of polycystic ovary syndrome and the risk of endometrial cancer: A mendelian randomization study. Front Endocrinol. 2021;12:e756137. https://doi.org/10.3389/fendo.2021.756137
Harris HR, Babic A, Webb PM, et al. Polycystic ovary syndrome, oligomenorrhea, and risk of ovarian cancer histotypes: Evidence from the ovarian cancer association consortium. Cancer Epidemiol Prevention Biomark. 2018;27(2):174-182. https://doi.org/10.1158/1055-9965
Schock H, Surcel HM, Zeleniuch-Jacquotte A, et al. Early pregnancy sex steroids and maternal risk of epithelial ovarian cancer. Endocrine-related Cancer. 2014;21(6):831-844. https://doi.org/10.1530/ERC-14-0282
Butler MS, Ricciardelli C, Tilley WD, Hickey TE. Androgen receptor protein levels are significantly reduced in serous ovarian carcinomas compared with benign or borderline disease but are not altered by cancer stage or metastatic progression. Hormon Cancer. 2013;4(3):154-164. https://doi.org/10.1007/s12672-013-0135-0
Gainder S, Sharma B. Update on management of polycystic ovarian syndrome for dermatologists. Indian Dermatol Online J. 2019;10(2):97-105. https://doi.org/10.4103/idoj.IDOJ_249_17
Acmaz G, Cınar L, Acmaz B, et al. The effects of oral isotretinoin in women with acne and polycystic ovary syndrome. Biomed Res Int. 2019;2019:e2513067. https://doi.org/10.1155/2019/2513067
Copyright (c) 2022 Saba Saeed

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










