Microbial Profile and Antimicrobial Resistance among the Most Common Grades of Diabetic Foot Ulcers (DFUs) at Mayo Hospital, Lahore, Pakistan
Abstract
 Abstract Views: 0
Abstract Views: 0
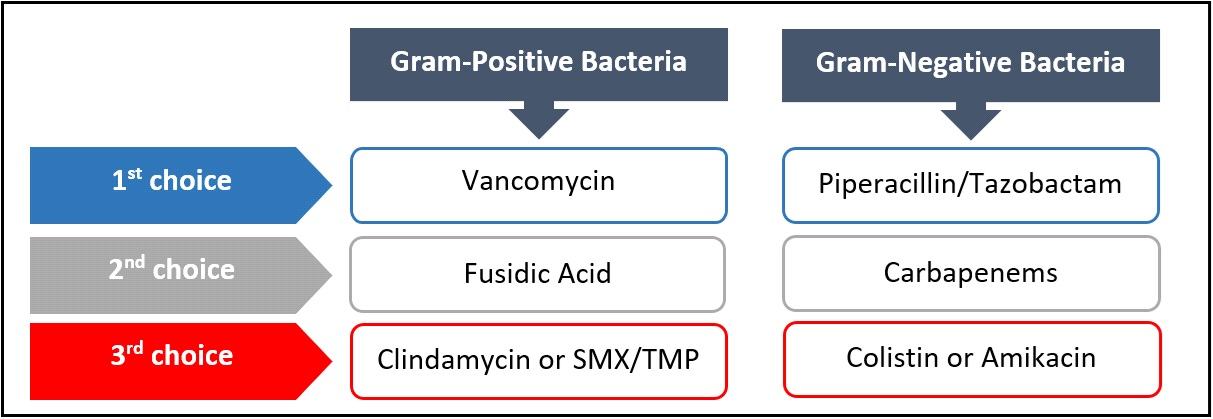
The current study was aimed to determine the pattern of antimicrobial resistivity of common microorganisms isolated from the most common grades of diabetic foot ulcers (DFUs) presenting at Mayo Hospital, Lahore, Pakistan. A total of 293 patients were included in the study conducted from January 2019 to December 2020. Deep-seated tissue samples of dimensions 0.5×0.5 cm were taken from the ulcer after surgical debridement, washed with saline, and immediately sent to the laboratory for culture and sensitivity (C&S). Data were analyzed by using SPSS 26. Grade 2 and Grade 3 DFUs (26.62% and 49.14%, respectively) were the most abundant of all DFUs, while Staphylococcus aureus was the most abundant bacteria. The polymicrobial growth pattern was found to be dominant in the current study. The incidence of MRSA was 68.4%(26/38) and 66.2%(49/74) in grades 2 and 3, respectively. The overall incidence of gram-negative microbes increased with an increase in the grade of ulcer. Hence, it can be concluded that early identification and grading of the disease can assist in the early initiation of empirical treatment and may reduce the unwanted morbidity of the disease. Furthermore, ultimate treatment should always be based on culture and sensitivity reported to minimize the disease's socioeconomic burden and morbidity.
Downloads
References
Magliano DJ, Boyko EJ, Atlas ID. What is diabetes? 10th ed. International Diabetes Federation; 2021. IDF DIABETES ATLAS. 10th edition
Mapa-Tassou C, Katte J-C, Maadjhou CM, Mbanya JC. Economic impact of diabetes in Africa. Curr Diabetes Rep. 2019;19:1–8. https://doi.org/10.1007/s11892-019-1124-7
Noor S, Raghav A, Parwez I, Ozair M, Ahmad J. Molecular and culture based assessment of bacterial pathogens in subjects with diabetic foot ulcer. Diabetes Metab Syndr. 2018;12(3):417–42 https://doi.org/10.1016/j.dsx.2018.03.001
Siddiqui MA, Naeem H, Ali MM, Randhawa FA, Nazir S, Farooqui F. Microbiological and antimicrobial pattern of diabetic foot ulcers (DFUs) at a tertiary care center in North East, Punjab. J Pak Med Assoc. 2021;71(6):1566–1569. https://doi.org/10.47391/JPMA. 1180
Miyan Z, Fawwad A, Sabir R, Basit A. Microbiological pattern of diabetic foot infections at a tertiary care center in a developing country. J Pak Med Assoc. 2017;53:10–20.
Kaimkhani GM, Siddiqui AA, Rasheed N, et al. Pattern of infecting microorganisms and their susceptibility to antimicrobial drugs in patients with diabetic foot infections in a tertiary care hospital in Karachi, Pakistan. Cureus. 2018;10(6):e2872. https://doi.org/10.7759/cureus.2872
Macdonald KE, Boeckh S, Stacey HJ, Jones JD. The microbiology of diabetic foot infections: a meta-analysis. BMC Infectious Dis. 2021;21(1):e770. https://doi.org/10.1186/s12879-021-06516-7
Siddiqui MA, Naeem H, Ali MM, Randhawa FA, Nazir S, Farooqui F. Microbiological and antimicrobial pattern of diabetic foot ulcers (DFUs) at a tertiary care center in North East, Punjab. J Pak Med Assoc. 2021;71(6):1566–1569. https://doi.org/10.47391/JPMA. 1180
Kwon KT, Armstrong DG. Microbiology and antimicrobial therapy for diabetic foot infections. Infect Chemother. 2018;50(1):11–20. https://doi.org/10.3947/ic.2018.50.1.11
Saseedharan S, Sahu M, Chaddha R, et al. Epidemiology of diabetic foot infections in a reference tertiary hospital in India. Braz J Microbiol. 2018;49(2):401–406. https://doi.org/10.1016/j.bjm.2017.09.003
Goh TC, Bajuri MY, Nadarajah SC, Rashid AHA, Baharuddin S, Zamri KS. Clinical and bacteriological profile of diabetic foot infections in a tertiary care. J Foot Ankle Res. 2020;13(1):e36. https://doi.org/10.1186/s13047-020-00406-y
Mougakou E, Mastrogianni E, Kyziroglou M. The role of novel antibiotics in the management of diabetic foot infection. Diabetes Ther. 2022;14:251–263. https://doi.org/10.1007/s13300-022-01357-2
Castro-Sánchez E, Moore LS, Husson F, Holmes AH. What are the factors driving antimicrobial resistance? Perspectives from a public event in London, England. BMC Infect Dis. 2016;16(1):e465. https://doi.org/10. 1186/s12879-016-1810-x
Monteiro-Soares M, Russell D, Boyko EJ, Jeffcoate WJ, Mills JL, Morbach S. IWGDF Guideline on the classification of diabetic foot ulcers. Diabetes Metab Res Rev. 2019.
Shabhay A, Horumpende P, Shabhay Z, et al. Clinical profiles of diabetic foot ulcer patients undergoing major limb amputation at a tertiary care center in North-eastern Tanzania. BMC Surg. 2021;21:e34. https://doi.org/10.1186/s12893-021-01051-3
Gul A, Basit A, Ali SM, Ahmadani MY, Miyan Z. Role of wound classification in predicting the outcome of diabetic foot ulcer. J Pak Med Assoc. 2006;56(10):444–447.
Hindler JF, Stelling J. Analysis and presentation of cumulative antibiograms: a new consensus guideline from the Clinical and Laboratory Standards Institute. Clinic Infect Dis. 2007;44(6):867–873. https://doi.org/10.1086/511864
Al Benwan K, Al Mulla A, Rotimi VO. A study of the microbiology of diabetic foot infections in a teaching hospital in Kuwait. J Infect Public Health. 2012;5(1):1–8. https://doi.org/10.1016/j.jiph.2011.07.004
McGrath R, Al Snih S, Markides K, Hall O, Peterson M. The burden of health conditions for middle-aged and older adults in the United States: disability-adjusted life years. BMC Geriatr. 2019;19:e100. https://doi.org/10.1186/s12877-019-1110-6
Wu WX, Liu D, Wang YW, et al. Empirical antibiotic treatment in diabetic foot infection: a study focusing on the culture and antibiotic sensitivity in a population from southern China. Int J Low Extrem Wounds. 2017;16(3):173–182. https://doi.org/10.1177/1534734617725410
Najari HR, Karimian T, Parsa H, QasemiBarqi R, Allami A. Bacteriology of moderate-to-severe diabetic foot infections in two tertiary hospitals of Iran. Foot. 2019;40:54–58. https://doi.org/10.1016/j.foot.2019.05.001
Wu M, Pan H, Leng W, Lei X, Chen L, Liang Z. Distribution of microbes and drug susceptibility in patients with diabetic foot infections in Southwest China. J Diabetes Res. 2018;2018:e9817308. https://doi.org/10.1155/2018/9817308
Bravo-Molina A, Linares-Palomino JP, Lozano-Alonso S, Asensio-García R, Ros-Díe E, Hernández-Quero J. Influence of wound scores and microbiology on the outcome of the diabetic foot syndrome. J Diabetes Complicat. 2016;30(2):329–334. https://doi.org/10.1016/j.jdiacomp.2015.11.001
Xie X, Bao Y, Ni L, et al. Bacterial profile and antibiotic resistance in patients with diabetic foot ulcer in Guangzhou, Southern China: Focus on the differences among different wagner's grades, IDSA/IWGDF grades, and ulcer types. Int J Endocrinol. 2017;2017:e8694903. https://doi.org/10.1155/2017/8694903
Jouhar L, Minhem M, Akl E, Rizk N, Hoballah J. Microbiological profile of diabetic foot infection in the Middle East and North Africa: a systematic review. Wounds. 2019;6(1):43–50.
Bansal E, Garg A, Bhatia S, Attri AK, Chander J. Spectrum of microbial flora in diabetic foot ulcers. Indian J Pathol Microbiol. 2008;51(2):204–208.
Lipsky BA, Aragón‐Sánchez J, Diggle M, et al. IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes. Diabetes Metab. Res. Rev. 2016;32:45–74. https://doi.org/10.1002/dmrr.2699
Copyright (c) 2023 Hamza Naeem, Sarfaraz Khan, Muhammad Arshad Siddiqui, Muhammad Mohsin Ali, Shahida Nazir Siddiqui, Amna Ghafoor, Sarmad Zahoor, Hafiz Mudabbar Mahboob

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










