Association of Age and Gender with the BMI of Obese Individuals in Lahore, Pakistan
Abstract
 Abstract Views: 197
Abstract Views: 197
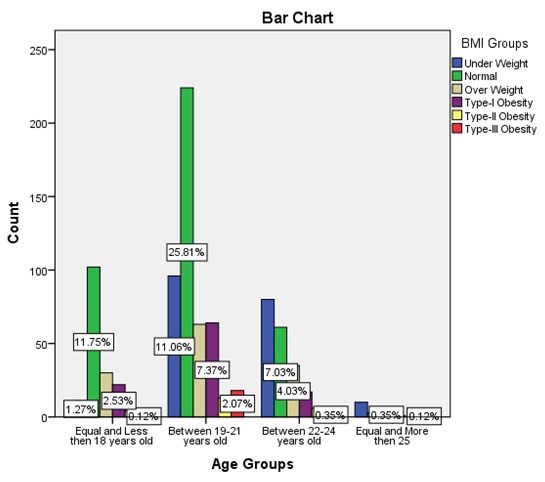
Obesity is a serious public health concern. It is expanding exponentially across the globe and is associated with chronic diseases, such as Type II diabetes and cardiovascular diseases. The aim of the current study was to find the association among age, gender, and Body Mass Index (BMI) of obese individuals residing in Lahore, Pakistan. This cross-sectional study was carried out in January 2021. Data was collected through an electronic questionnaire. A total of 868 individuals (84.3% female and 15.7% male) of ages between 18 to 60 years participated in the current study. Convenient sampling method was used. Anthropometrics including weight, height, and age were taken in kilograms (kg), centimeters (cm) and years, respectively. The standard equation to calculate BMI was used (weight in kg/height in m²). WHO BMI cut-points for Asians were used to assess the BMI status of the selected individuals. Statistical analysis was carried out through Microsoft Excel and SPSS. It was found that the prevalence of obesity was 17.2% (12% Type I obesity, while 2.6% Type II and Type III obesity), while 15.1% participants were found to be overweight, 22.7% were underweight, and 44.9% were determined to be normal. It was also determined that the prevalence of underweight, overweight, Type I, Type II, and Type III obesity is more common among women (20.6%, 12.3%, 9.2%, 2.3%, and 2%, respectively) than men (2.1%, 2.8%, 2.8%, 0.3%, and 0.7%, respectively) (p-value <0.05), indicating a positive association. The highest prevalence of underweight, overweight, Type I, Type II, and Type III obesity was observed in age group 19-21 years (11.1%, 7.3%, 7.4%, 1.5%, and 2.1%, respectively) (p-value <0.05). These results would help to develop public health programs and preventive measures to reduce the prevalence of the above risk factors for obesity and other non-communicable diseases.
Downloads
References
Zhu Y, Wang Z, Maruyama H, Onoda K, Huang Q. Body fat percentage and normal-weight obesity in the Chinese population: Development of a simple evaluation indicator using anthropometric measurements. Int. J. Environ. Res. Public Health. 2022;19(7):e4238. https://doi.org/10.3390/ijerph19074238
Sturm R. Increases in morbid obesity in the USA: 2000-2005. Public Health. 2007;121(7):492-496. https://doi.org/10.1016/j.puhe.2007.01.006
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6-10. https://doi.org/10.1016/j.metabol.2018.09.005
Kopelman PG. Obesity as a medical problem. Nature. 2000;404(6778):635-643. https://doi.org/10.1038/35007508
Zhou S, Ye B, Fu P, et al. Double burden of malnutrition: Examining the growth profile and coexistence of undernutrition, overweight, and obesity among school-aged children and adolescents in urban and rural counties in Henan province, China. J Obes. 2020;2020:e2962138. https://doi.org/10.1155/2020/2962138
Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89(6):2583-2589. https://doi.org/10.1210/jc.2004-0535
Katsiki N, Anagnostis P, Kotsa K, Goulis DG, Mikhailidis DP. Obesity, metabolic syndrome and the risk of microvascular complications in patients with diabetes mellitus. Curr Pharm Des. 2019;25(18):2051-2059. https://doi.org/10.2174/1381612825666190708192134
Jih J, Mukherjea A, Vittinghoff E, et al. Using appropriate body mass index cut points for overweight and obesity among Asian Americans. Prev Med. 2014;65:1-6. https://doi.org/10.1016/j.ypmed.2014.04.010
Phillips CM. Metabolically healthy obesity: definitions, determinants and clinical implications. Rev Endocr Metab Disord. 2013;14(3):219-227. https://doi.org/10.1007/s11154-013-9252-x
Hou Q, Guan Y, Yu W, et al. Associations between obesity and cognitive impairment in the Chinese elderly: an observational study. Clin Interv Aging. 2019;14:367-373. https://doi.org/10.2147/CIA.S192050
Bowman K, Thambisetty M, Kuchel GA, Ferrucci L, Melzer D. Obesity and longer term risks of dementia in 65-74 Year Olds. Age Ageing. 2019;48(3):367-373. https://doi.org/10.1093/ageing/afz002
Silventoinen K, Sans S, Tolonen H, et al. Trends in obesity and energy supply in the WHO MONICA Project. Int J Obes Relat Metab Disord. 2004;28(5):710-718. https://doi.org/10.1038/sj.ijo.0802614
Church T, Martin CK. The obesity epidemic: A consequence of reduced energy expenditure and the uncoupling of energy intake? Obesity (Silver Spring). 2018;26(1):14-16. https://doi.org/10.1002/oby.22072
Oussaada SM, van Galen KA, Cooiman MI, et al. The pathogenesis of obesity. Metabolism. 2019;92:26-36. https://doi.org/10.1016/j.metabol.2018.12.012
Wang JB, Patterson RE, Ang A, Emond JA, Shetty N, Arab L. Timing of energy intake during the day is associated with the risk of obesity in adults. J Hum Nutr Diet. 2014;27 Suppl 2:255-262. https://doi.org/10.1111/jhn.12141
Ma Y, He FJ, MacGregor GA. High salt intake: Independent risk factor for obesity? Hypertension. 2015;66(4):843-849. https://doi.org/10.1161/HYPERTENSIONAHA.115.05948
Zhou L, Stamler J, Chan Q, et al. Salt intake and prevalence of overweight/obesity in Japan, China, the United Kingdom, and the United States: the INTERMAP Study. Am J Clin Nutr. 2019;110(1):34-40. https://doi.org/10.1093/ajcn/nqz067
Klingbeil E, de La Serre CB. Microbiota modulation by eating patterns and diet composition: impact on food intake. Am J Physiol Regul Integr Comp Physiol. 2018;315(6):R1254-R1260. https://doi.org/10.1152/ajpregu.00037.2018
Jais A, Paeger L, Sotelo-Hitschfeld T, et al. PNOCARC Neurons Promote Hyperphagia and Obesity upon High-Fat-Diet Feeding. Neuron. 2020;106(6):1009-1025. https://doi.org/10.1016/j.neuron.2020.03.022
Chou S, Rashad I, Grossman M. Fast‐Food Restaurant Advertising on Television and Its Influence on Childhood Obesity. The Journal of Law & Economics.2008;51(4):599–618. https://doi.org/10.1086/590132
Seth B, Arora S, Singh R. Association of obesity with hormonal imbalance in infertility: a cross-sectional study in north Indian women. Indian J Clin Biochem. 2013;28(4):342-347. https://doi.org/10.1007/s12291-013-0301-8
Zargar AH, Masoodi SR, Laway BA, et al. Prevalence of obesity in adults--an epidemiological study from Kashmir Valley of Indian Subcontinent. J Assoc Physicians India. 2000;48(12):1170-1174.
Biritwum R, Gyapong J, Mensah G. The epidemiology of obesity in ghana. Ghana Med J. 2005;39(3):82-85.
Popkin BM, Conde W, Hou N, Monteiro C. Is there a lag globally in overweight trends for children compared with adults?. Obesity (Silver Spring). 2006;14(10):1846-1853. https://doi.org/10.1038/oby.2006.213
Mushtaq MU, Gull S, Khurshid U, Shahid U, Shad MA, Siddiqui AM. Prevalence and socio-demographic correlates of stunting and thinness among Pakistani primary school children. BMC Public Health. 2011;11:e790. https://doi.org/10.1186/1471-2458-11-790
Misra A, Dhurandhar NV. Current formula for calculating body mass index is applicable to Asian populations. Nutr Diabetes. 2019;9(1):e3. https://doi.org/10.1038/s41387-018-0070-9
Zatterale F, Longo M, Naderi J, et al. Chronic adipose tissue inflammation linking obesity to insulin resistance and Type 2 diabetes. Front Physiol. 2020;10:1607. https://doi.org/10.3389/fphys.2019.01607
Lee CH, Lam KS. Obesity-induced insulin resistance and macrophage infiltration of the adipose tissue: A vicious cycle. J Diabetes Investig. 2019;10(1):29-31. https://doi.org/10.1111/jdi.12918
Jakobsen GS, Småstuen MC, Sandbu R, et al. Association of bariatric surgery vs medical obesity treatment with long-term medical complications and obesity-related comorbidities. JAMA. 2018;319(3):291-301. https://doi.org/10.1001/jama.2017.21055
Idrees M, Poverty in Pakistan: A region-specific analysis. Lahore J Econom. 2017;22(2):139-163. https://doi.org/10.35536/lje.2017.v22.i2.a6
Aslam R, Sharif F, Baqar M, Nizami AS, Ashraf U. Role of ambient air pollution in asthma spread among various population groups of Lahore City: A case study. Environ Sci Pollut Res. https://doi.org/10.1007/s11356-022-19086-1
Peltzer K, Pengpid S, Samuels TA, et al. Prevalence of overweight/obesity and its associated factors among university students from 22 countries. Int J Environ Res Public Health. 2014;11(7):7425-7441. https://doi.org/10.3390/ijerph110707425
Tanzil S, Jamali T. Obesity, An emerging epidemic in Pakistan-a review of evidence. J Ayub Med Coll Abbottabad. 2016;28(3):597-600.
Asif M, Aslam M, Altaf S, Atif S, Majid A. Prevalence and Sociodemographic Factors of Overweight and Obesity among Pakistani Adults. J Obes Metab Syndr. 2020 Mar 30;29(1):58-66. doi: 10.7570/jomes19039. PMID: 32045513; PMCID: PMC7118000.
Copyright (c) 2022 Faheem Mustafa

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










