Effects of Nutrition Education Program on Lactating Mothers in Relation to Infant Feeding Practices
Abstract
 Abstract Views: 0
Abstract Views: 0
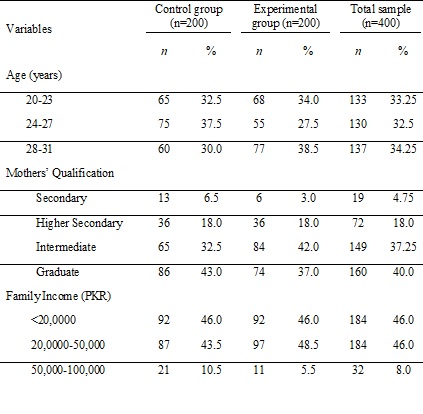
Maternal and child health status is profoundly affected by infant feeding practices. In Pakistan, these practices are sub optimal which may lead to adverse outcomes. The initiation of breastfeeding within the first hour of birth, as well as good counseling of lactating mothers regarding infant weaning and introduction of complementary foods to the infants in a hygienic and clean environment, can decrease the risk of malnutrition and infections, leading to a decrease in infant morbidity and mortality. Increasing the awareness of mothers regarding recommended feeding practices is a key to improving this situation, especially in the region of South Asia. The current study was conducted with the aim of assessing the impacts of contextually developed nutrition education sessions on the knowledge and attitudes of women regarding infant feeding. A quasi experiment was conducted for this purpose. A sample of 400 lactating mothers between 20-30 years of age visiting a private post-natal clinic located in Lahore, Pakistan was selected. Half of the sample (200) was included in the experimental group and exposed to 12 weeks of educational intervention based on various audio-visual aids. Pretest and posttest knowledge and attitude scores of the women of both control and experimental groups were recorded. The results showed that women belonging to both control and experimental groups had similar knowledge regarding infant feeding at baseline (pretest). However, experimental group showed significant improvement in knowledge scores after intervention, as compared to control. The results also revealed that simple educational intervention can lead to profound improvements in maternal knowledge and attitudes regarding infant feeding. Increasing awareness is the first step in the translation of knowledge into practice. Therefore, similar interventions may be helpful in improving infant breast and complementary feeding practices. Effective implementation of nutrition education interventions that can improve the breastfeeding rates and also bring about improvement in complementary feeding practices is important for a developing country like Pakistan. This, in turn, may lead to better health outcomes for infants by reducing direct and indirect impacts of undernutrition.
Downloads
References
Pretorius CE, Asare H, Genuneit J, Kruger HS, Ricci C. Impact of breastfeeding on mortality in sub-Saharan Africa: a systematic review, meta-analysis, and cost-evaluation. Eur J Pediatr. 2020;179:1213–1225. https://doi.org/10.1007/s00431-020-03721-5
Martin M, Blackwell A, Kaplan H, Gurven M. Differences in Tsimane children’s growth outcomes and associated determinants as estimated by WHO standards vs. within-population references. PLOS ONE. 2019;14(4):e0214965. https://doi.org/10.1371/journal.pone.0214965
Alpers B, Blackwell V, Clegg ME. Standard v. baby-led complementary feeding: a comparison of food and nutrient intakes in 6–12-month-old infants in the UK. Public Health Nutr. 2019;22(15):2813–2822. https://doi.org/10.1017/S136898001900082X
Cardenas SD, Puello SD, Montes LA. Breastfeeding and related factors in afrodescendant women from Cartagena, Colombia. Pesqui Bras Odontopediatria Clín Integr. 2020;20:e5359. https://doi.org/10.1590/pboci.2020.049
Amir S, Sherazi N, Tanweer A. Maternal nutrition education as a tool to optimize the Infant feeding practices-a narrative review. Innt Med Health Sci. 2022;2(1):36–42.
Taki S, Russell CG, Lymer S, et el. A mixed methods study to explore the effects of program design elements and participant characteristics on parents' engagement with an mHealth program to promote healthy infant feeding: the growing healthy program. Front Endocrinol. 2019;10:e397. https://doi.org/10.3389/fendo.2019.00397
Tchuimi DT. Does maternal empowerment influence childhood stunting and wasting in Cameroon? a cross-sectional study. Vulner Child Youth Stud. 2023;18(2):263–281. https://doi.org/10.1080/17450128.2022.2141405
Olatona FA, Adeniyi DB, Obrutu OE, Ogunyemi AO. Nutritional knowledge, dietary habits and nutritional status of adults living in urban communities in Lagos State. Afr Health Sci. 2023;23(1):711–724. https://doi.org/10.4314/ahs.v23i1.76
Helle C, Hillesund ER, Wills AK, Øverby NC. Examining the effects of an eHealth intervention from infant age 6 to 12 months on child eating behaviors and maternal feeding practices one year after cessation: The Norwegian randomized controlled trial early food for future health. PLOS ONE. 2019;14(8):e0220437.
Arikpo D, Edet ES, Chibuzor MT, Odey F, Caldwell DM. Educational interventions for improving primary caregiver complementary feeding practices for children aged 24 months and under. Cochrane Database Syst Rev. 2018(5). https://doi.org/10.1002/14651858.CD011768.pub2
Ross E, Munoz FM, Edem B, et al. Failure to thrive: case definition & guidelines for data collection, analysis, and presentation of maternal immunisation safety data. Vaccine. 2017;35(48Part A):6483– 6491. https://doi.org/10.1016/j.vaccine.2017.01.051
Shrestha S, Pokhrel M, Mathema S. Knowledge, attitude and practices among mothers of children 6 to 24 months of age regarding complementary feeding. JNMA J Nepal Med Assoc. 2020;58(230):758–763. https://doi.org/10.31729/jnma.5274
Girard AW, Waugh E, Sawyer S, Golding L, Ramakrishnan U. A scoping review of social‐behaviour change techniques applied in complementary feeding interventions. Matern Child Nutr. 2020;16(1):e12882. https://doi.org/10.1111/mcn.12882
Mahumud RA, Uprety S, Wali N, Renzaho AM, Chitekwe S. The effectiveness of interventions on nutrition social behaviour change communication in improving child nutritional status within the first 1000 days: evidence from a systematic review and meta‐analysis. Matern Child Nutr. 2022;18(1):e13286. https://doi.org/10.1111/mcn.13286
Chopel A, Soto D, Joiner BJ, et al. Multilevel factors influencing young mothers’ breastfeeding: a qualitative CBPR study. J Hum Lact. 2019;35(2):301–317. https://doi.org/10.1177/0890334418812076
Heidkamp RA, Piwoz E, Gillespie S, et al. Mobilising evidence, data, and resources to achieve global maternal and child undernutrition targets and the Sustainable Development Goals: an agenda for action. Lancet. 2021;397(10282):1400–1418. https://doi.org/10.1016/S0140-6736(21)00568-7
Jardí C, Casanova BD, Arija V. Nutrition education programs aimed at african mothers of infant children: A systematic review. Int J Environ Res Pub Health. 2021;18(14):e7709. https://doi.org/10.3390/ijerph18147709
McFadden A, Gavine A, Renfrew MJ, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev. 2017;(2):eCD001141. https://doi.org/10.1002/14651858.CD001141.pub5
Colecraft EK, Christian AK, Ammah G, Aryeetey R. Rapid review of research on dietary attitudes, beliefs and practices in Ghana 1990-2020. Afr J Food Agri Nutr Develop. 2022;22(2):19417–19440.
Asher RC, Shrewsbury VA, Bucher T, Collins CE. Culinary medicine and culinary nutrition education for individuals with the capacity to influence health related behaviour change: a scoping review. J Human Nutr Diet. 2022;35(2):388–395. https://doi.org/10.1111/jhn.12944
Copyright (c) 2023 Naima Shirazi, Asma Afreen, Mahnaz Nasir Khan

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










