Evaluating the Risk Factors and Bidirectional Association of Urinary Tract Infections in Diabetes Mellitus
Abstract
 Abstract Views: 0
Abstract Views: 0
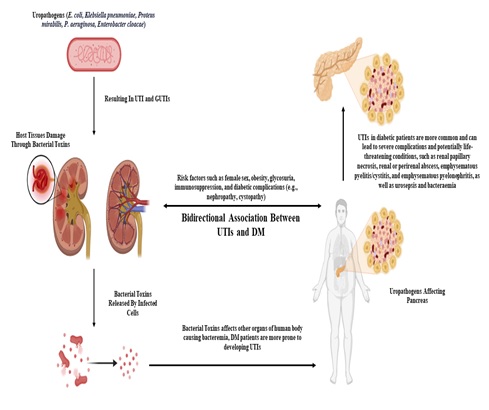
Background. Urinary tract infections (UTIs) are the most predominant among people with diabetes mellitus (DM), with significant implications for morbidity and mortality. Various microbial agents, including bacteria, fungi, and viruses, contribute to UTIs in diabetic patients.
Objective. This review aims to examine the association between UTIs and DM, focusing on pathogenic mechanisms, risk factors, and clinical implications.
Methods. A comprehensive literature review was conducted to gather data on UTIs in diabetic patients. Relevant articles gathered from various databases, such as PubMed, Google Scholar, Semantic Scholar, and ScienceDirect were analyzed for insights into microbial colonization, pathogenic mechanisms, and epidemiological trends.
Results. Microorganisms commonly implicated in diabetic UTIs include Escherichia coli, Proteus mirabilis, Enterobacter spp., and Klebsiella spp. Elevated urinary glucose levels provide a conducive environment for microbial growth, contributing to increased infection rates. Risk factors such as female sex, obesity, glycosuria, immunosuppression, and diabetic complications (such as nephropathy and cystopathy) further exacerbate susceptibility.
Conclusion. The incidence of UTIs in diabetic populations is rising globally, provoked by antibiotic resistance among uropathogens such as Gram-negative bacteria including Escherichia coli (65-80%), trailed by Pseudomonas aeruginosa, Proteus mirabilis (2-6%), and Klebsiella spp. (3.5-13%). Whereas, Gram-positive bacteria include Staphylococcus spp. (4-6%), GBS (3%), Enterococcus faecalis (4-7%), and Candida (1%).
Downloads
References
Kash MS, Rehman K, Fiayyaz F, Sabir S, Khurshid M. Diabetes-associated infections: development of antimicrobial resistance and possible treatment strategies. Arch Microbiol. 2020;202(5):953–965. https://doi.org/10.1007/s00203-020-01818-x
Kumar R, Kumar R, Perswani P, Taimur M, Shah A, Shaukat F. Clinical and microbiological profile of urinary tract infections in diabetic versus non-diabetic individuals. Cureus. 2019;11(8):e5464. https://doi.org/10.7759/cureus.5464
Niveditha S, Pramodhini S, Umadevi S, Kumar S, Stephen S. The isolation and the biofilm formation of uropathogens in the patients with catheter associated urinary tract infections (UTIs). J Clinic Diag Res. 2012;6(9):1478–1482. https://doi.org/10.7860/JCDR/2012/4367.2537
Stapleton A. Urinary tract infections in patients with diabetes. Am J Med. 2002. 113(1):80–84. https://doi.org/10.1016/S0002-9343(02)01062-8
Woldemariam HK, Geleta DA, Tulu KD, et al. Common uropathogens and their antibiotic susceptibility pattern among diabetic patients. BMC Infect Dis. 2019;19(1):e43. https://doi.org/10.1186/s12879-018-3669-5
La Vignera S, Condorelli RA, Cannarella R, et al. Urogenital infections in patients with diabetes mellitus: Beyond the conventional aspects. Int J Immunopathol Pharmacol. 2019;33:1–6. https://doi.org/10.1177/2058738419866582
Ramrakhia S, Raja K, Dev K, Kumar A, Kumar V, Kumar B. Comparison of incidence of urinary tract infection in diabetic vs non-diabetic and associated pathogens. Cureus. 2020;12(9):e10500. https://doi.org/10.7759/cureus.10500
Pragash DS, Girija S, Sekar U, Rayapu V, Sheriff D. Uropathogens and diabetes mellitus-a perspective. IOSR J Dent Med Sci. 2017;16(5):29–32.
Mody L, Juthani-Mehta M. Urinary tract infections in older women: a clinical review. JAMA. 2014;311(8):844–854. https://doi.org/10.1001/jama.2014.303
Worku GY, Alamneh YB, Abegaz WE. Prevalence of bacterial urinary tract infection and antimicrobial susceptibility patterns among diabetes mellitus patients attending Zewditu memorial hospital, Addis Ababa, Ethiopia. Infect Drug Resist. 2021;14:1441–1454.
Bissong ME, Fon PN, Tabe-Besong FO, Akenji TN. Asymptomatic bacteriuria in diabetes mellitus patients in Southwest Cameroon. Afr Health Sci. 2013;13(3):661–666. https://doi.org/10.4314/ahs.v13i3.20
López-de-Andrés A, Albaladejo-Vicente R, Palacios-Ceña D, et al. Time trends in spain from 2001 to 2018 in the incidence and outcomes of hospitalization for urinary tract infections in patients with type 2 diabetes mellitus. Int J Environ Res Public Health. 2020:17(24):e9427. https://doi.org/10.3390/ijerph17249427
Fu AZ, Iglay K, Qiu Y, Engel S, Shankar R, Brodovicz K. Risk characterization for urinary tract infections in subjects with newly diagnosed type 2 diabetes. J Diabet Complic. 2014;28(6):805–810. https://doi.org/10.1016/j.jdiacomp.2014.06.009
Nabaigwa BI, Mwambi B, Okiria J, Oyet C. Common uropathogens among diabetic patients with urinary tract infection at Jinja Regional Referral Hospital, Uganda. Afr J Laborat Med. 2018;7(1):1–3.
Sanden AK, Johansen MB, Pedersen L, Lervang HH, Schønheyder HC, Thomsen RW. Change from oral antidiabetic therapy to insulin and risk of urinary tract infections in Type 2 diabetic patients: a population-based prescription study. J Diabet Complic. 2010;24(6):375–381. https://doi.org/10.1016/j.jdiacomp.2010.01.002
Borowczyk M, Chmielarz-Czarnocińska A, Faner-Szczepańska P, et al. Urinary tract infections in postmenopausal women with type 2 diabetes: clinical correlates and quinolone susceptibility. Pol Arch Intern Med. 2017;127(5):305–307. https://doi.org/10.20 452/pamw.4019
Hamdan HZ, Kubbara E, Adam AM, Hassan OS, Suliman SO, Adam I. Urinary tract infections and antimicrobial sensitivity among diabetic patients at Khartoum, Sudan. Ann Clinic Microbiol Antimicrob, 2015;14:e26. https://doi.org/10.1186/s12941-015-0082-4
Wang MC, Tseng CC, Wu AB, et al. Bacterial characteristics and glycemic control in diabetic patients with Escherichia coli urinary tract infection. J Microbiol Immunol Infect. 2013;46(1):24–29. https://doi.org/10.1016/j.jmii.2011.12.024
Mama M, Manilal A, Gezmu T, Kidanewold A, Gosa F, Gebresilasie A. Prevalence and associated factors of urinary tract infections among diabetic patients in Arba Minch Hospital, Arba Minch province, South Ethiopia. Turk J Urol. 2019;45(1):56–62. https://doi.org/10.5152/tud.2018.32855
Sewify M, Nair S, Warsame S, Murad M, Alhubail A, Behbehani K, Al-Refaei F, Tiss A. Prevalence of urinary tract infection and antimicrobial susceptibility among diabetic patients with controlled and uncontrolled glycemia in Kuwait. J Dia Res. 2016;2016(1):e6573215. https://doi.org/10.1155/2016/6573215
Borj M, Taghizadehborojeni SI, Shokati AM, et al. Urinary tract infection among diabetic patients with regard to the risk factors, causative organisms and their antimicrobial susceptibility profiles at Firoozgar Hospital, Tehran, Iran. Int J Life Sci Pharm Res. 2017;7(3):L38–L47.
Geerlings SE. Urinary tract infections in patients with diabetes mellitus: epidemiology, pathogenesis and treatment. Int J Antimicrob Agent. 2008;31:54–57. https://doi.org/10.1016/j.ijantimicag.2007.07.042
Popejoy MW, Long J, Huntington JA. Analysis of patients with diabetes and complicated intra-abdominal infection or complicated urinary tract infection in phase 3 trials of ceftolozane/tazobactam. BMC Infect Dis. 2017;17(1):e316. https://doi.org/10.1186/s12879-017-2414-9
Dave VR, Shah VR, Sonaliya KN, Shah SD, Gohel AR. A study on epidemiological profile of urinary tract infections in perspective of diabetic status among patients attending Tertiary Care Hospital, Ahmedabad. Natl J Commun Med. 2018;9:594–598.
Geerlings S, Fonseca V, Castro-Diaz D, List J, Parikh S. Genital and urinary tract infections in diabetes: impact of pharmacologically-induced glucosuria. Diab Res Clinic Pract. 2014;103(3):373–381. https://doi.org/10.1016/j.diabres.2013.12.052
Ampaire L, Butoto A, Orikiriza P, Muhwezi O. Bacterial and drug susceptibility profiles of urinary tract infection in diabetes mellitus patients at Mbarara Regional Referral hospital, Uganda. Microbiol Res J Int. 2015;9(4):eBMRJ.17483.
Geerlings SE, Stolk RP, Camps MJ, et al. Asymptomatic bacteriuria can be considered a diabetic complication in women with diabetes mellitus. In: Emoődy L, Pál T, Hacker J, Blum-Oehler G, eds. Genes and Proteins Underlying Microbial Urinary Tract Virulence: Basic Aspects and Applications. Springer; 2002:309–314.
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–284. https://doi.org/10.1038/nrmicro3432
Wagenlehner FM, Johansen TEB, Cai T, et al. Epidemiology, definition and treatment of complicated urinary tract infections. Nat Rev Urol. 2020;17(10):586–600. https://doi.org/10.1038/s41585-020-0362-4
Hakeem LM, Bhattacharyya DN, Lafong C, Janjua KS, Serhan JT, Campbell IW. Diversity and complexity of urinary tract infection in diabetes mellitus. Brit J Diabet Vascul Dis. 2009;9(3):119–125. https://doi.org/10.1177/1474651409105654
Pishdad R, Auwaerter PG, Kalyani RR. Diabetes, SGLT-2 Inhibitors, and Urinary Tract Infection: a review. Curr Diab Rep. 2024;24(5):108–117. https://doi.org/10.1007/s11892-024-01537-3
Ipe DS, Sundac L, Benjamin WH, Jr., Moore KH, Ulett GC. Asymptomatic bacteriuria: prevalence rates of causal microorganisms, etiology of infection in different patient populations, and recent advances in molecular detection. FEMS Microbiol Lett. 2013;346(1):1–10. https://doi.org/10.1111/1574-6968.12204
Delamaire M, Maugendre D, Moreno M, Le Goff MC, Allannic H, Genetet B. Impaired leucocyte functions in diabetic patients. Diabet Med. 1997;14(1):29–34. https://doi.org/10.1002/(SICI)1096-9136(199701)14:1%3C29::AID-DIA300%3E3.0.CO;2-V
Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nat Rev Endocrinol. 2012;8(4):228–236. https://doi.org/10.1038/nrendo.2011.183
Hosking DJ, Bennett T, Hampton JR. Diabetic autonomic neuropathy. Diabetes. 1978;27(10):1043–1054. https://doi.org/10.2337/diab.27.10.1043
Shriyan HC. Clinical and Microbiological Profile of Urinary Tract Infection in Diabetic and Nondiabetic Patients [Doctoral dissertation]. Karnataka, India: Shri Dharmasthala Manjunatheshwara University; 2022
Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Ind J Endocrinol Metabol. 2012;16(Suppl1):S27–S36. https://doi.org/10.4103/2230-8210.94253
Peleg AY, Weerarathna T, McCarthy JS, Davis TM. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabet/Metabol Res Rev. 2007;23(1):3–13. https://doi.org/10.1002/dmrr.682
Karslıoğlu M, Yılmaz MO. Exploring the nexus: prevalence, risk factors, and clinical correlations of urinary tract infections in diabetes mellitus patients-a comprehensive retrospective analysis. Anatol Curr Med J. 2024;6(1):93–96. https://doi.org/10.38053/acmj.1402336
Shahsavari S, Bakht M, Sadeghi H, et al. The effect of diabetes mellitus on the spectrum of uropathogens and the antimicrobial resistance in patients with urinary tract infection. Arch Razi Inst. 2024;79(1):92–101.
Shalgam DO, Al-Tamimi BAAA, Dhaif SS, Salman SB, Salman IN. Escherichia col resistance in type 2 diabetes mellitus with Urinary Tract Infection (UTI). Stall J Multidiscip Associat Res Stud. 2024;3(3):69–73. https://doi.org/10.55544/sjmars.3.3.9
Soteropoulos C, Kawashima E, Gilmore JH. Cystitis and ureteritis emphysematosa. Radiology. 1957;68(6):866–868. https://doi.org/10.1148/68.6.866
Bailey H. Cystitis emphysematosa; 19 case with intraluminal and interstitial collections of gas. Am J Roentogen. 1961;86:850–862.
Rosenberg JW, Quader A, Brown JS. Renal emphysema. Urology. 1973;1(3):237–239. https://doi.org/10.1016/0090-4295(73)90743-7
Roy C, Pfleger DD, Tuchmann CM, Lang HH, Saussine CC, Jacqmin D. Emphysematous pyelitis: findings in five patients. Radiology. 2001;218(3):647–650. https://doi.org/10.1148/radiology.218.3.r01fe14647
Bobba RK, Arsura EL, Sarna PS, Sawh AK. Emphysematous cystitis: an unusual disease of the genito-urinary system suspected on imaging. Ann Clinic Microbiol Antimicrob. 2004;3:e20. https://doi.org/10.1186/1476-0711-3-20
Thomas AA, Lane BR, Thomas AZ, Remer EM, Campbell SC, Shoskes DA. Emphysematous cystitis: a review of 135 cases. BJU Int. 2007;100(1):17–20. https://doi.org/10.1111/j.1464-410X.2007.06930.x
Pontin AR, Barnes RD. Current management of emphysematous pyelonephritis. Nat Rev Urol. 2009;6(5):272–279. https://doi.org/10.1038/nrurol.2009.51
Eid YM, Salam MM. Diabetic ketoacidosis presenting with emphysematous pyelonephritis. J Diabet Complic. 2010;24(3):214–216. https://doi.org/10.1016/j.jdiacomp.2008.12.010
Li L, Parwani AV. Xanthogranulomatous pyelonephritis. Arch Pathol Laborat Med. 2011;135(5):671–674. https://doi.org/10.5858/2009-0769-RSR.1
Jia H, Su W, Zhang J, Wei Z, Tsikwa P, Wang Y. Risk factors for urinary tract infection in elderly patients with type 2 diabetes: a protocol for systematic review and meta-analysis. Plos One. 2024;19(9):e0310903. https://doi.org/10.1371/journal.pone.0310903
Nishikawara M, Harada M, Yamazaki D, Kakegawa T, Hashimoto K, Kamijo Y. A case of emphysematous pyelonephritis in an older man with poorly controlled type 2 diabetes mellitus. CEN Case Rep. 2024;13(3):161–167. https://doi.org/10.1007/s13730-023-00821-7
Copyright (c) 2024 Haris Riaz Khan Khan, Naila Qamar

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










