Impact of Parental Vaccination Status on Yellow Fever Vaccination in Children Aged 0–1 Years in the Democratic Republic of Congo: Mixed Sequential Explanatory Study
Abstract
 Abstract Views: 0
Abstract Views: 0
Background. Yellow fever occurs in the intertropical regions of Africa and South America. Vaccination is a simple, effective, and inexpensive means to reduce morbidity and mortality from infectious diseases. Presently, the world is witnessing a decrease in the number of children vaccinated each year in low-income countries and in the Democratic Republic of the Congo (DRC). This scenario is leading towards concrete consequences and even a resurgence of vaccine-preventable infectious diseases.
Methodology. This is a sequential and explanatory study conducted using a mixed-method approach. The quantitative component, of the retrospective, multicenter, analytical type, was carried out using data from the post-campaign yellow fever coverage study in 8 concerned provinces. Whereas the qualitative component, of the descriptive phenomenological type, was carried out through semi-directive interviews held with the heads of household of children aged 0-1 year in Tshuapa Province. Quantitative data was analyzed using SPSS (version 25) and qualitative data was analyzed using ATLAS-Ti 22 software.
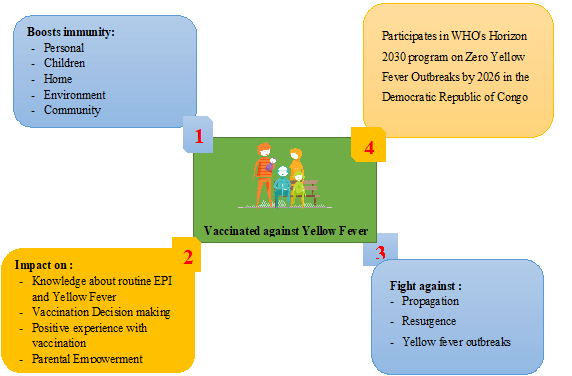
Results. Quantitative analysis showed that there was a statistically significant influence of the household head's vaccination status on the routine vaccination of children aged 0–1 year, with a chi-square test indicating χ2=62.706 and p=0.000. This means that children whose parents are immunized are more likely to be immunized as well. Despite this positive influence, the study revealed that 27.7% of immunized children had parents who were themselves immunized. This figure raises concerns about the effectiveness of awareness campaigns and parental decision-making on immunization. Qualitative analysis highlighted several factors influencing parental decision to vaccinate including parents' knowledge of vaccination, their positive experiences with it, and their sense of parental responsibility.
Conclusion. These results highlight not only the importance of household heads' vaccination status in the child immunization process, however, also the need to address concerns related to immunized children, even in households where parents are immunized. Therefore, national authorities must develop effective strategies to improve immunization coverage and raise family awareness regarding the importance of vaccination.
Downloads
References
Yellow fever. Ministère du travail, de la santé et des solidarités de la France Web site. https://sante.gouv.fr/soins-et-maladies/maladies/maladies-infectieuses/la-fievre-jaune. Updated February 25, 2025. Accessed March 7, 2024.
Yellow fever. Pan American Health Organization Web site. https://www.paho.org/en/topics/yellow-fever. Accessed December 5, 2023.
Yellow fever - African Region (AFRO). WHO Web site. https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON510. Updated March 20, 2024. Accessed January 29, 2025.
Carlson R. Yellow fever outbreaks cause 11% case fatality rate. Vax Before Travel Web site. https://www.vax-before-travel.com/yellow-fever-outbreaks-cause-11-case-fatality-rate-2024-03-20. Updated March 20, 2024. Accessed January 29, 2025.
Yellow fever risk areas. Fit for Travel Website.https://www.fitfortravel.nhs.uk/advice/disease-prevention-advice/yellow-fever/yellow-fever-risk-areas. Accessed January 29, 2025.
Définition de vaccination. Centre National de Ressources Textuelles et Lexicales Web site. https://www.cnrtl.fr/definition/vaccination. Accessed April 7, 2024.
Nissen C. The age limits of healthy childhood and youth. Trib Santé. 2023;77(3):27-38. https://doi.org/10.3917/seve1.077.0027
UNICEF. Multiple indicator cluster survey, 2017-2018, survey results report. Kinshasa, Democratic Republic of Congo, MICS-Palu 2018. https://www.unicef.org/drcongo/media/3646/file/cod-mics-palu-2018.pdf. Published December, 2019.
Organisation Mondiale de la Santé. Agenda for immunization 2030: a global strategy to leave no one behind. https://www.who.int/fr/publications/m/item/immunization-agenda-2030-a-global-strategy-to-leave-no-one-behind. Updated April 1, 2020. Accessed April 7, 2024.
Lindsey NP, Horton J, Barrett AD, et al. Yellow fever resurgence: an avoidable crisis? Npj Vaccines. 2022;7(1):e137. https://doi.org/10.1038/s41541-022-00552-3
Vaccination in low-income countries: pandemic has led to decline in coverage but signs of recovery are emerging. ReliefWeb Web site. https://reliefweb.int/report/world/vaccination-dans-les-pays-faible-revenu-la-pandemie-entraine-une-baisse-de-la-couverture-mais-des-signes-de-reprise-commencent-poindre. Updated July 29, 2022. Accessed August 31, 2022.
Dropping vaccination rates in Democratic Republic of Congo could lead to resurgence of deadly diseases. UNICEF Web site. https://www.unicef.org/drcongo/communiques-presse/baisse-taux-vaccination-resurgence-maladies-mortelles. Updated May 15, 2020. Accessed March 7, 2024.
Ribau C, Lasry JC, Bouchard L, Moutel G, Hervé C, Marc-Vergnes JP. Phenomenology: a scientific approach to lived experiences. Rech Soins Infirm. 2005;81(2):21-27.
Broomé RE. Descriptive phenomenological psychological method: an example of a methodology section from doctoral dissertation. https://tinyurl.com/fwf7d4v6. Published November, 2011.
Giorgi AP, Giorgi BM. The descriptive phenomenological psychological method. In: Camic PM, Rhodes JE, Yardley L, eds. Qualitative Research in Psychology: Expanding Perspectives in Methodology and Design. American Psychological Association. 2003:243-273.
Giorgi A. Psychology as a Human Science: A Phenomenologically Based Approach. University Professors Press; 2020.
Giorgi A. Sketch of a psychological phenomenological method. In: Phenomenology and Psychological Research. Duquesne University Press; 1985:8-22.
Giorgi A. The Descriptive Phenomenological Method in Psychology: A Modified Husserlian Approach. Duquesne University Press; 2009.
Wertz FJ. The descriptive phenomenological method in psychology: a modified Husserlian approach. J Phenomenol Psychol. 2010;41(2):269-276.
Giorgi A. Convergence and divergence of qualitative and quantitative methods in psychology. Duquesne Stud Phenomenol Psychol. 1975;2:72-79. https://doi.org/10.5840/dspp197528
Reasons to vaccinate. CDC Web site. https://www.cdc.gov/vaccines/parents/why-vaccinate/vaccine-decision.html. Updated March 7, 2023. Accessed December 5, 2023.
Gérard EEM, Bien-Aimé MM, Marcelin NM, et al. Post-Yellow fever vaccination coverage survey in the provinces of Mongala, Tshuapa, Bas-Uele, Haut-Uele, Nord-Ubangi, Sud-Ubangi and Tshopo of the Democratic Republic of Congo in 2021. Glob Sci J. 2022;10(2):1584-1600.
World Health Organization. Global strategy for the elimination of yellow fever epidemics (?EYE)? 2017-2026. https://apps.who.int/iris/handle/10665/272955. Updated June 27, 2018. Accessed October 1, 2022.
Minta AA, Ferrari M, Antoni S, et al. Progress towards regional measles elimination - worldwide, 2000-2021. Center for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/71/wr/mm7147a1.htm. Updated November 25, 2022. Accessed April 7, 2024.
Rachlin A, Danovaro-Holliday MC, Murphy P, Sodha SV, Wallace AS. Routine vaccination coverage - Worldwide, 2021. MMWR Morbid Mortal Weekly Rep. 2022;71(44):1396-1400. https://doi.org/10.15585/mmwr.mm7144a2
Mbengue MAS, Sarr M, Faye A, et al. Determinants of complete immunization among senegalese children aged 12-23 months: evidence from the demographic and health survey. BMC Public Health. 2017;17(1):e630. https://doi.org/10.1186/s12889-017-4493-3
Ngalamulume AK, Banayi LK, Ndimba BS, Kalemba M, Zambi KM. Explanatory factors for low vaccination coverage in children aged 0 to 11 months in the Luiza Zs, DRC: risks and perception of mothers. Int J Soc Sci Sci Stud. 2022;2(6):1402-1421.
Immunization coverage. WHO Web site. https://www.who.int/news-room/fact-sheets/detail/immunization-coverage. Updated July 15, 2022. Accessed November 2, 2022.
Fadnes LT, Jackson D, Engebretsen IM, et al. Vaccination coverage and timeliness in three South African areas: a prospective study. BMC Public Health. 2011;11(1):e404. https://doi.org/10.1186/1471-2458-11-404
Lakew Y, Bekele A, Biadgilign S. Factors influencing full immunization coverage among 12-23 months of age children in Ethiopia: evidence from the national demographic and health survey in 2011. BMC Public Health. 2015;15:e728. https://doi.org/10.1186/s12889-015-2078-6
Bekondi C, Zanchi R, Seck A, et al. HBV immunization and vaccine coverage among hospitalized children in Cameroon, Central African Republic and Senegal: a cross-sectional study. BMC Infect Dis. 2015;15(1):e267. https://doi.org/10.1186/s12879-015-1000-2
Djafar MA, Moumouni K, Aboubacar S, Aissata HG, Garba M, Alido S. Determinant of the vaccination status of infants under 12 months hospitalized in two national hospitals ofNiamey. J Pédiatrie Puériculture. 2022;35(1):21-28. https://doi.org/10.1016/j.jpp.2021.12.007
Bicaba A, Rawlings B, Ouedraogo B. The Acceptability And Feasibility Of Introducing The Standard Days Method (SDM) Of Family Planning In Reproductive Health Clinics In Burkina Faso West Africa. Final Report. USAID; 2005.
Asfaw AG, Koye DN, Demssie AF, Zeleke EG, Gelaw YA. Determinants of default to fully completion of immunization among children aged 12 to 23 months in south Ethiopia: unmatched case-control study. Pan Afr Med J. 2016;23:e100. https://doi.org/10.11604/pamj.2016.23.100.7879
Abadura SA, Lerebo WT, Kulkarni U, Mekonnen ZA. Individual and community level determinants of childhood full immunization in Ethiopia: a multilevel analysis. BMC Public Health. 2015;15:e972. https://doi.org/10.1186/s12889-015-2315-z
Antai D. Inequitable childhood immunization uptake in Nigeria: a multilevel analysis of individual and contextual determinants. BMC Infect Dis. 2009;9(1):e181. https://doi.org/10.1186/1471-2334-9-181
Wiysonge CS, Uthman OA, Ndumbe PM, Hussey GD. Individual and contextual factors associated with low childhood immunisation coverage in sub-Saharan Africa: a multilevel analysis. PloS One. 2012;7(5):e37905. https://doi.org/10.1371/journal.pone.0037905
Zaidi SMA, Khowaja S, Dharma VK, Khan AJ, Chandir S. Coverage, timeliness, and determinants of immunization completion in Pakistan: evidence from the Demographic and Health Survey (2006-07). Hum Vaccines Immunother. 2014;10(6):1712-1720. https://doi.org/10.4161/hv.28621
Sangare Y, Kone K, Diarra A, et al. Etude comparative des déterminants psychosociaux de la vaccination anti-poliomylite à Kabalabougou et Sangarebougou. Rev Malienne Sci Technol. 2020;1(23):46-55.
Lernout T, Theeten H, Hens N, et al. Timeliness of infant vaccination and factors related with delay in Flanders, Belgium. Vaccine. 2014;32(2):284-289. https://doi.org/10.1016/j.vaccine.2013.10.084
Bobossi-Serengbé G, Fioboy R, Ndoyo J, Nakouné E. Missed opportunities for immunization in children of 0 to 11 monthsin Bangui. J Pédiatrie Puériculture. 2014;27(6):289-293. https://doi.org/10.1016/j.jpp.2014.08.010
MacDonald NE, Dubé E. Nouvelle ressource permettant de résumer les données sur la vaccination provenant du Centre canadien de ressources et d'échange sur les données probantes en vaccination (CANVax). Relevé Mal Transm Au Can. 2020;46(1):17-21. https://doi.org/10.14745/ccdr.v46i01a03f
Bégué P. Le refus des vaccinations. Aspects actuels en 2012 et solutions en santé publique. Bull Académie Natl Médecine. 2012;196(3):603-618.
MacDonald NE, Dubé E. Nouvelle ressource permettant de résumer les données sur la vaccination provenant du Centre canadien de ressources et d’échange sur les données probantes en vaccination (CANVax). Relevé Mal Transm Au Can. 2020;46(1):17-21. http://doi.org/10.14745/ccdr.v46i01a03f
Bégué P. Le refus des vaccinations. Aspects actuels en 2012 et solutions en santé publique. Bull Académie Natl Médecine. 2012;196(3):603-618.
Copyright (c) 2025 ABRAHAM MUKONGO BULAIMU LUKEBA, Gerard Eloko Eya Matangelo, Simon-Decap Mabakutuvangilanga Ntela, Monique Rothan- Tondeur, Rita Georges Nohra

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










