Prevalence, In Silico Analysis and Possible Molecular Drug Therapy for Specific Meningitis Types
Abstract
 Abstract Views: 0
Abstract Views: 0
Background. Meningitis is the inflammation of the membranes surrounding the brain and spinal cord. This study was designed to determine the prevalence of meningitis along with the docking of bacterial proteins with drugs used to treat meningitis.
Methodology. A cross-sectional study was conducted including 100 febrile seizure children admitted to the hospitals of Hyderabad, Pakistan. Demographic data was recorded via a questionnaire. Cerebrospinal fluid (CSF) and blood were analyzed clinically. Molecular docking via PyRx―a virtual screening tool―was performed and Chi-square test was applied to interpret the data.
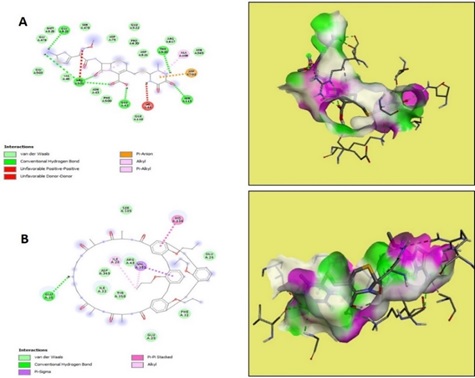
Results. Out of the 100 patients included in the study, 32 had been diagnosed with meningitis, 53 were suspected patients, and 15 were patients of encephalitis. Among diagnosed meningitis patients, 47% had bacterial meningitis, 16% had viral meningitis, while only 9% had TBM. Moreover, 28% of patients were partially treated with a mortality rate of 18%. Low glucose levels, high protein levels, and high neutrophil count were found in cerebrospinal fluid (CSF). The majority of patients were vaccinated (48%). Meningitis was more frequent among infant children and the results were statistically significant (p-value = 0.01). Molecular docking revealed that ceftriaxone had the greatest affinity for bacterial proteins, while Haemophilus influenza Hia Adhesin (3syj) and Pneumolysin (5aoe) had the lowest Kd values of -9 and -8.6, respectively.
Conclusion. Bacterial meningitis was found to be the most prevalent type with 32% prevalence. Ceftriaxone could be the drug of choice if meningitis is caused by 3syj or 5aoe. However, either vancomycin or meropenem may be preferred over ceftriaxone if meningitis is caused by 1p4t (Neisserial surface protein A).
Downloads
References
Eilbert W, Chan C. Febrile seizures: a review. J Am Coll Emerg Phys Open. 2022;3:e12769. https://doi.org/10.1002/emp2.12769
do Valle DA, Costa LCV, Fregonese AP, et al. Characteristics and risk factors of central nervous system infection in children with febrile seizures. Pediatr Emerg Care. 2023;40(6):438–442. https://doi.org/10.1097/PEC.0000000000003158
Ali SA, Taj MK, Ali SH. Antimicrobial resistance pattern of bacterial meningitis among patients in Quetta, Pakistan. Infect Drug Resist. 2021;14:5107–5120. https://doi.org/10.2147/IDR.S339231
Tsang RS. A narrative review of the molecular epidemiology and laboratory surveillance of vaccine preventable bacterial meningitis agents: streptococcus pneumoniae, neisseria meningitidis, haemophilus influenzae and streptococcus agalactiae. Microorganisms. 2021;9:e449. https://doi.org/10.3390/microorganisms9020449
Jiang H, Su M, Kui L, et al. Prevalence and antibiotic resistance profiles of cerebrospinal fluid pathogens in children with acute bacterial meningitis in Yunnan province, China, 2012-2015. PloS One. 2017;12(6):e0180161. https://doi.org/10.1371/journal.pone.0180161
Petersen PT, Bodilsen J, Jepsen MPG, et al. Clinical features and prognostic factors in adults with viral meningitis. Brain. 2023;146:3816–3825. https://doi.org/10.1093/brain/awad089
Mustafa A, Mustafa A, Rahman RU, Iqbal R, Parkash O, Siddiqui A. Frequency of meningitis in children aged 06 months to 59 months presenting with first episode of fits with fever in pediatric emergency department. Pak J Med Health Sci. 2023;17(5):578–580. https://doi.org/10.53350/pjmhs2023175578
Feldman C, Anderson R. Meningococcal pneumonia: a review. Pneumonia. 2019;11:e3. https://doi.org/10.1186/s41479-019-0062-0
Zwahlen M, Stute P. Impact of progesterone on the immune system in women: a systematic literature review. Arch Gynecol Obst. 2024;309:37–46. https://doi.org/10.1007/s00404-023-06996-9
Kwambana-Adams B. Global burden of meningitis and implications for strategy. Lancet Neurol. 2023;22:646–648. https://doi.org/10.1016/S1474-4422(23)00244-2
Madaki UY, Shu’aibu A, Umar MI. Mathematical model for the dynamics of bacterial meningitis (Meningococcal meningitis): a case study of Yobe State Specialist Hospital, Damaturu, Nigeria. Gadau J Pure Allied Sci. 2023;2(2):113–29. https://doi.org/10.54117/gjpas.v2i2.19
Audshasai T, Coles JA, Panagiotou S, et al. Streptococcus pneumoniae rapidly translocate from the nasopharynx through the cribriform plate to invade the outer meninges. Mbio. 2022;13:e01024-22. https://doi.org/10.1128/mbio.01024-22
Mohanty T, Fisher J, Bakochi A, et al. Neutrophil extracellular traps in the central nervous system hinder bacterial clearance during pneumococcal meningitis. Nature Commun. 2019;10:e1667. https://doi.org/10.1038/s41467-019-09040-0
Zhang C, Tan Z, Tian F. Impaired consciousness and decreased glucose concentration of CSF as prognostic factors in immunocompetent patients with cryptococcal meningitis. BMC Infect Dis. 2020;20:e69. https://doi.org/10.1186/s12879-020-4794-5
Panji M, Behmard V, Raoufi MF, et al. Evaluation of biological markers in children's cerebrospinal fluid with bacterial and viral meningitis. Int J Med Labor. 2023;10(3):208–216. https://doi.org/10.18502/ijml.v10i3.13745
Shah Sa, Mallah Fa, Mari Ar, Tahira K, Amjad M, Khan A. Incidence and causative organisms of acute bacterial meningitis, our hospital experience. Pak J Med Health Sci. 2022;15(12):e3852-6. https://doi.org/10.53350/pjmhs2115123852
Abdulaziz ATA, Li J, Zhou D. The prevalence, characteristics and outcome of seizure in tuberculous meningitis. Acta Epileptol. 2020;2:e1. https://doi.org/10.1186/s42494-020-0010-x
Castilla J, Cenoz MG, Abad R, et al. Effectiveness of a meningococcal group B vaccine (4CMenB) in children. New Eng J Med. 2023;388(5):427–438. https://doi.org/10.1056/NEJMoa2206433
Garai P, Atack JM, Wills BM, Jennings MP, Bakaletz LO, Brockman KL. Adherence of nontypeable haemophilus influenzae to cells and substrates of the airway is differentially regulated by individual modA phasevarions. Microbiol Spect. 2023;11(1):e04093-22. https://doi.org/10.1128/spectrum.04093-22
Yee W-X, Barnes G, Lavender H, Tang CM. Meningococcal factor H-binding protein: implications for disease susceptibility, virulence, and vaccines. Trends Microbiol. 2023;31(8):805–815. https://doi.org/10.1016/j.tim.2023.02.011
Copyright (c) 2024 Beenish Khanzada, Abdul wasay Memon, Rida e Zehra Syeda, Samra Khan Bhand

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










