Effects of Preloading with High Dose of Atorvastatin Prior to Percutaneous Coronary Intervention: A Single Center Randomized Controlled Trial
Abstract
 Abstract Views: 0
Abstract Views: 0
Background. Percutaneous coronary intervention (PCI) establishes the blood flow back to the heart. However, it can damage myocardium, leading to various cardiovascular events. Atorvastatin have beneficial pleiotropic cardiovascular effects, in addition to their lipid-lowering effects. Little work has been conducted with regard to its preloading in developing countries. This study aimed to analyze the effects of statin preloading in patients undergoing PCI in terms of reduction in major adverse cardiovascular events (MACE).
Methodology. This randomized controlled study was conducted at the Punjab Institute of Cardiology, Lahore for 6 months. A total of 186 patients undergoing elective PCI were included through non-probability consecutive sampling. Informed consent and demographic information were obtained. Two groups were formed, that is, the experimental group (receiving 80 mg atorvastatin prior to PCI) and the control group (not receiving atorvastatin before PCI). All patients were followed up at the intervals of 24 hours, 48 hours, and 1 month. MACE was calculated and data was analyzed in SPSS 26.0.
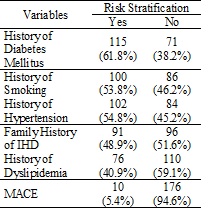
Results. The current study showed that the average age of participants was 55.10 ± 8.69 (age range 32-71 years). A total of 155 (83.33%) male participants and 31 (16.67%) female participants were enrolled for the study. Among the participants, there were 115 (61.8%) patients with diabetes mellitus, 102 (54.8%) with hypertension, 76 (40.9%) with dyslipidemia, and 91(48.9%) had a history of IHD. There were 10 patients who had major cardiovascular events. So, MACE came out to be 5.4%. Comparing both the groups, there were 2/93 (2.1%) patients in the experimental group who had MACE, whereas 8/93 (8.6%) patients had MACE in the control group. This difference was not statistically significant (p-value = 0.1).
Conclusion. Atorvastatin preloading before PCI reduces MACE by improving the perfusion of the myocardium.
Downloads
References
Severino P, D’Amato A, Pucci M, et al. Ischemic heart disease pathophysiology paradigms overview: from plaque activation to microvascular dysfunction. Int J Molecul Sci. 2020;21(21):e8118. https://doi.org/10.3390/ijms21218118
Safiri S, Karamzad N, Singh K, et al. Burden of ischemic heart disease and its attributable risk factors in 204 countries and territories, 1990–2019. Eur J Prevent Cardiol. 2022;29(2):420–431. https://doi.org /10.1093/eurjpc/zwab213
Montrief T, Davis WT, Koyfman A, Long B. Mechanical, inflammatory, and embolic complications of myocardial infarction: an emergency medicine review. Am J Emerg Med. 2019;37(6):1175–1183. https://doi. org/10.1016/j.ajem.2019.04.003
Duggan JP, Peters AS, Trachiotis GD, Antevil JL. Epidemiology of coronary artery disease. Surg Clinics. 2022;102(3):499–516. https://doi.org /10.1016/j.suc.2022.01.007
Raza Q, Nicolaou M, Dijkshoorn H, Seidell JC. Comparison of general health status, myocardial infarction, obesity, diabetes, and fruit and vegetable intake between immigrant Pakistani population in the Netherlands and the local Amsterdam population. Ethnic Health. 2017;22(6):551–564. https://doi.org/ 10.1080/13557858.2016.1244741
Hara H, Serruys PW, Takahashi K, et al. Impact of peri-procedural myocardial infarction on outcomes after revascularization. J Am College Cardiol. 2020;76(14):1622–1639.
Riaz A, Hanif MI, Khan IH, Hanif A. Frequency and causes of periprocedural myocardial infarction in complex coronary interventions. Pak Heart J. 2019;52(2):137–143.
Sinan UY, Meric BK, Bursa N, Moumin G, Kaya A, Ozkan AA. Evaluation of preprocedural statin loading on clinical outcomes in patients undergoing elective percutaneous coronary intervention. Front Cardiovascul Med. 2024;11:e1435989. https://doi.org/10 .3389/fcvm.2024.1435989
Choudhary A, Rawat U, Kumar P, Mittal P. Pleotropic effects of statins: the dilemma of wider utilization of statin. Egyp Heart J. 2023;75(1):e1. https://doi.org/10.1186/s43044-023-00327-8
Ahmed Z, Shaiea S, Zeng H. Clinical outcomes of different atorvastatin loading dose before selective percutaneous coronary intervention. Int J Dental Med Sci Res. 2020;4(5):1–9.
Berwanger O, Santucci EV, de Andrade Jesuíno I, et al. Effect of loading dose of atorvastatin prior to planned percutaneous coronary intervention on major adverse cardiovascular events in acute coronary syndrome: the SECURE-PCI randomized clinical trial. JAMA. 2018;319(13):1331–1340. https://doi. org/10.1001/jama.2018.2444
Lampropoulos K, Megalou A, Bazoukis G, Tse G, Manolis A. Pre‐loading therapy with statins in patients with angina and acute coronary syndromes undergoing PCI. J Interven Cardiol. 2017;30(6):507–513. https://doi.org/10.1111/joic.12421
Alkhouli M, Alqahtani F, Kalra A, et al. Trends in characteristics and outcomes of hospital inpatients undergoing coronary revascularization in the United States, 2003-2016. JAMA Network Open. 2020;3(2):e1921326. https://doi.org/10.1001/jamanetworkopen.2019.21326
Zhao L, Li S, Gao Y. Efficacy of statins on renal function in patients with chronic kidney disease: a systematic review and meta-analysis. Renal Fail. 2021;43(1):718–728. https://doi.org/10.1080/0886022X.2021.1915799
Pan Y, Tan Y, Li B, Li X. Efficacy of high-dose rosuvastatin preloading in patients undergoing percutaneous coronary intervention: a meta-analysis of fourteen randomized controlled trials. Lipids Health Dis. 2015;14:e97. https://doi.org/10.1186/s12944-015-0095-1
Anayat S, Majid K, Nazir HS, et al. Meta-analysis on the efficacy of high-dose statin loading before percutaneous coronary intervention in reducing no-reflow phenomenon in acute coronary syndrome. Am J Cardiol. 2023;195:9–16. https://doi. org/10.1016/j.amjcard.2023.02.024
Elserafy AS, Farag NM, El Desoky AI, Eletriby KA. Effect of high-intensity statin preloading on TIMI flow in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Egypt Heart J. 2020;72:e40. https://doi.org/10. 1186/s43044-020-00074-0
Ma M, Bu L, Shi L, et al. Effect of loading dose of atorvastatin therapy prior to percutaneous coronary intervention in patients with acute coronary syndrome: a meta-analysis of six randomized controlled trials. Drug Desig Develop Ther. 2019;13:1233–1240.
Borovac JA, Leth-Olsen M, Kumric M, et al. Efficacy of high-dose atorvastatin or rosuvastatin loading in patients with acute coronary syndrome undergoing percutaneous coronary intervention: a meta-analysis of randomized controlled trials with GRADE qualification of available evidence. Eur J Clinic Pharmacol. 2022;78:111–1126. https://doi.org /10.1007/s00228-021-03196-9
Dewi LP, Yogiarto RM, Suryawan IG, Pratama MD. The effect of atorvastatin administration before percutaneous coronary intervention on stable coronary artery disease against event of periprocedural myocardial infarction. In: IOP Conference Series: Earth and Environmental Science. IOP Publishing; 2020:e012191.
Newman CB, Preiss D, Tobert JA, et al. Statin safety and associated adverse events: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2019;39(2):e38–e81. https://doi.org/10.1161/ATV.0000000000000073
Copyright (c) 2024 Sarmad Zahoor, Samra Yasmin, Zia ur Rehman, Hafiz Mudabbar Mahboob, Muhammad Ali Khawaja, Sadia Iqbal, Sadia Iqbal

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










