Antibacterial Susceptibility Patterns of UTI Pathogens among Different Age Groups in Lahore, Pakistan
Abstract
 Abstract Views: 0
Abstract Views: 0
Background. Urinary tract infections (UTIs) are a significant health problem. They affect individuals across all age groups globally, with a higher prevalence among women and patients with chronic disorders such as diabetes.
Methodology. The current study was performed in the Department of Urology at The University of Lahore to explore the susceptibility of UTIs across different age groups in this region. For this purpose, 157 patients presented with the symptoms of frequent urination and pain during urination were considered. These also included some patients admitted in The University of Lahore Teaching Hospital. Midstream urine samples were collected from patients and cultured. Bacterial colonies of positive cultures were identified through morphological characteristics and serological tests such as Lancefield grouping. Additionally, biochemical tests and API 20E were used to identify members of the Enterobacteriaceae family. The data was analyzed using SPSS (version 25.0).
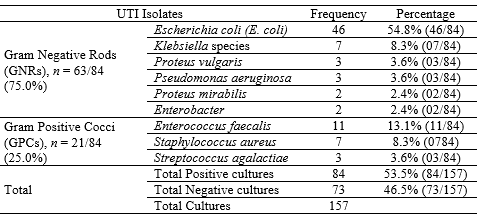
Results. In this study, the overall prevalence of UTIs was 53.5%, with the highest incidence of UTIs occurring in patients aged 25 to 45 years. The frequently identified isolates comprised Escherichia coli which accounted for 46 (54.8%) cases, followed by Enterococcus species accounting for 11 (13.1%) cases, Klebsiella species accounting for 07 (8.3%) cases, and Staphylococcus aureus accounting for another 07 (8.3%) cases. Furthermore, it was found that gram-negative bacteria showed a high level of resistance with 73.3% for cefixime, 73.2% for ceftriaxone, 73.0% for ceftazidime, and a relatively low level of resistance against fosfomycin (15.9%) and nitrofurantoin (16.3%). On the other hand, gram-positive isolates showed a higher level of resistance against penicillin (66.7%). Whereas, all isolates were found to be sensitive to gentamycin (100%).
Conclusion. Routine antimicrobial susceptibility testing prior to antibiotic prescription is recommended. Aminoglycosides, fosfomycin, and nitrofurantoin proved to be the most effective drugs of choice against these bacteria.
Downloads
References
Zhao F, Yang H, Bi D, Khaledi A, Qiao M. A systematic review and meta-analysis of antibiotic resistance patterns, and the correlation between biofilm formation with virulence factors in uropathogenic E. coli isolated from urinary tract infections. Microb Pathog. 2020;144:e104196. https://doi.org/10.1016/j.micpath.2020.104196
Zagaglia C, Ammendolia MG, Maurizi L, Nicoletti M, Longhi C. Urinary tract infections: the current scenario and future prospects. Pathogens. 2023;12(4):e623. https://doi.org/10.3390/pathogens12040623
Zagaglia C, Ammendolia MG, Maurizi L, Nicoletti M, Longhi C. Urinary tract infections caused by Uropathogenic Escherichia coli strains–new strategies for an old pathogen. Microorganisms. 2022;10(7):e1425. https://doi.org/10.3390/microorganisms10071425
Zeng Z, Zhan J, Zhang K, Chen H, Cheng S. Global, regional, and national burden of urinary tract infections from 1990 to 2019: an analysis of the global burden of disease study 2019. World J Urol. 2022;40(3):755–763. https://doi.org/10.1007/s00345-021-03913-0
Grigoryan L, Mulgirigama A, Powell M, Schmiemann G. The emotional impact of urinary tract infections in women: a qualitative analysis. BMC Womens Health. 2022;22(1):e182. https://doi.org/10.1186/s12905-022-01757-3
Naber KG, Tirán-Saucedo J, Wagenlehner FME. Psychosocial burden of recurrent uncomplicated urinary tract infections. GMS Infect Dis. 2022;10:eDoc01. https://doi.org/10.3205/id000078
Czajkowski K, Broś-Konopielko M, Teliga-Czajkowska J. Urinary tract infection in women. Menopause Rev Menopauzalny. 2021;20(1):40–47. https://doi.org/10.5114/pm.2021.105382
Murray BO, Flores C, Williams C, et al. Recurrent urinary tract infection: a mystery in search of better model systems. Front Cell Infect Microbiol. 2021;11:691210. https://doi.org/10.3389/fcimb.2021.691210
Bader MS, Loeb M, Leto D, Brooks AA. Treatment of urinary tract infections in the era of antimicrobial resistance and new antimicrobial agents. Postgrad Med. 2020;132(3):234–250. https://doi.org/10.1080/00325481.2019.1680052
Klein RD, Hultgren SJ. Urinary tract infections: microbial pathogenesis, host–pathogen interactions and new treatment strategies. Nat Rev Microbiol. 2020;18(4):211–226. https://doi.org/10.1038/s41579-020-0324-0
Centers for Disease Control and Prevention. Urinary tract infection (catheter-associated urinary tract infection [CAUTI] and non-catheter-associated urinary tract infection [UTI]) events. https://www.cdc.gov/nhsn/pdfs/pscmanual/7psccauticurrent.pdf. Accessed October 15, 2024.
Abalkhail A, AlYami AS, Alrashedi SF, et al. The prevalence of multidrug-resistant Escherichia coli producing ESBL among male and female patients with urinary tract infections in Riyadh region, Saudi Arabia. Healthcare. 2022;10(9):e1778. https://doi.org/10.3390/healthcare10091778
Maharjan G, Khadka P, Shilpakar GS, Chapagain G, Dhungana GR. Catheter-associated urinary tract infection and obstinate biofilm producers. Can J Infect Dis Med Microbiol. 2018;2018(1):e7624857. https://doi.org/10.1155/2018/7624857
Teferi S, Sahlemariam Z, Mekonnen M, et al. Uropathogenic bacterial profile and antibiotic susceptibility pattern of isolates among gynecological cases admitted to Jimma Medical Center, South West Ethiopia. Sci Rep. 2023;13(1):e7078. https://doi.org/10.1038/s41598-023-34048-4
Uddin TM, Chakraborty AJ, Khusro A, et al. Antibiotic resistance in microbes: History, mechanisms, therapeutic strategies and prospects. J Infect Public Health. 2021;14(12):1750–1766. https://doi.org/10.1016/j.jiph.2021.10.020
Khan A, Saraf VS, Siddiqui F, et al. Multidrug resistance among uropathogenic clonal group A E. Coli isolates from Pakistani women with uncomplicated urinary tract infections. BMC Microbiol. 2024;24(1):e74. https://doi.org/10.1186/s12866-024-03221-8
Fatima S, Akbar A, Irfan M, et al. Virulence factors and antimicrobial resistance of Uropathogenic Escherichia coli eq101 UPEC isolated from UTI patient in Quetta, Baluchistan, Pakistan. BioMed Res Int. 2023;2023(1):e7278070. https://doi.org/10.1155/2023/7278070
Al-Shahrani GS, Belali TM. Frequency of drug-resistant bacterial isolates among pregnant women with UTI in maternity and children’s hospital, Bisha, Saudi Arabia. Sci Rep. 2024;14(1):e7397. https://doi.org/10.1038/s41598-024-58275-5
Morris CJ, Rohn JL, Glickman S, Mansfield KJ. Effective treatments of UTI—is intravesical therapy the future? Pathogens. 2023;12(3):e417. https://doi.org/10.3390/pathogens12030417
Nobel F, Akter S, Jebin R, et al. Prevalence of multidrug resistance patterns of Escherichia coli from suspected urinary tract infection in Mymensingh city, Bangladesh. J Adv Biotechnol Exp Ther. 2021;4(3):256–264. https://doi.org/10.5455/jabet.2021.d126
Rasool MS, Siddiqui F, Ajaz M, Rasool SA. Prevalence and antibiotic resistance profiles of gram negative bacilli associated with urinary tract infections (UTIs) in Karachi, Pakistan. Pak J Pharm Sci. 2019;32(6). https://doi.org/10.36721/PJPS.2019.32.6.REG.2617-2623.1
Roy R, Tiwari M, Donelli G, Tiwari V. Strategies for combating bacterial biofilms: a focus on anti-biofilm agents and their mechanisms of action. Virulence. 2018;9(1):522–554. https://doi.org/10.1080/21505594.2017.1313372
Zavala-Cerna MG, Segura-Cobos M, Gonzalez R, et al. The clinical significance of high antimicrobial resistance in community-acquired urinary tract infections. Can J Infect Dis Med Microbiol. 2020;2020(1):e2967260. https://doi.org/10.1155/2020/2967260
Mekonnen S, Tesfa T, Shume T, Tebeje F, Urgesa K, Weldegebreal F. Bacterial profile, their antibiotic susceptibility pattern, and associated factors of urinary tract infections in children at Hiwot Fana Specialized University Hospital, Eastern Ethiopia. PLOS ONE. 2023;18(4):e0283637. https://doi.org/10.1371/journal.pone.0283637
Dasgupta C, Rafi MA, Salam MA. High prevalence of multidrug-resistant uropathogens: A recent audit of antimicrobial susceptibility testing from a tertiary care hospital in Bangladesh. Pak J Med Sci. 2020;36(6):1297–1302. https://doi.org/10.12669/pjms.36.6.2943
Ahsan A, Zahra FT, Asif A, et al. Antibiotic resistance and virulence genes in Escherichia coli isolated from patients in a tertiary care hospital: implications for clinical management and public health. BioSci Rev. 2024;6(3):106–121. https://doi.org/10.32350/bsr.63.07
Bilal H, Khan MN, Rehman T, et al. Antibiotic resistance in Pakistan: a systematic review of past decade. BMC Infect Dis. 2021;21:e244. https://doi.org/10.1186/s12879-021-05906-1
Baunoch D, Luke N, Wang D, et al. Concordance between antibiotic resistance genes and susceptibility in symptomatic urinary tract infections. Infect Drug Resist. 2021;14:3275–3286. https://doi.org/10.2147/IDR.S323095
Toosky MN, Grunwald JT, Pala D, et al. A rapid, point-of-care antibiotic susceptibility test for urinary tract infections. J Med Microbiol. 2020;69(1):52–62. https://doi.org/10.1099/jmm.0.001119
Muhammad A, Khan SN, Ali N, Rehman MU, Ali I. Prevalence and antibiotic susceptibility pattern of uropathogens in outpatients at a tertiary care hospital. New Microbes New Infect. 2020;36:e100716. https://doi.org/10.1016/j.nmni.2020.100716
Ogodo AC, Agwaranze DI, Daji M, Aso RE. Chapter 13 - Microbial techniques and methods: basic techniques and microscopy. In: Egbuna C, Patrick-Iwuanyanwu KC, Shah MA, Ifemeje JC, Rasul A, eds. Analytical Techniques in Biosciences. Academic Press; 2022:201–220. https://doi.org/10.1016/B978-0-12-822654-4.00003-8
Karah N, Rafei R, Elamin W, et al. Guideline for urine culture and biochemical identification of bacterial urinary pathogens in low-resource settings. Diagnostics. 2020;10(10):e832. https://doi.org/10.3390/diagnostics10100832
Clinical and Laboratory Standards Institute. CLSI M100: Performance Standards for Antimicrobial Susceptibility Testing. Clinical and Laboratory Standards Institute; 2024.
Storme O, Saucedo JT, Garcia-Mora A, Dehesa-Dávila M, Naber KG. Risk factors and predisposing conditions for urinary tract infection. Ther Adv Urol. 2019;11:e1756287218814382. https://doi.org/10.1177/1756287218814382
Ejaz SM, Vohra MS, Raza Y. Prevalence and antibiotic susceptibility pattern of isolates from patients with urinary tract infection in Karachi. Microbiol Immunol Commun. 2022;1(1):7–19. https://doi.org/10.55627/mic.001.01.0179
Ahmad S, Ali F, Qureshi S, et al. The evaluation of antibiotic susceptibility pattern and associated risk factors of UTI in tertiary care hospital of Peshawar. Pak J Pharm Sci. 2022;35:897–903. https://doi.org/10.36721/PJPS.2022.35.3.SP.897-903.1
Asim A, Javed R, Aziz A, et al. Incidence of culture proven UTI and antimicrobial sensitivity pattern among the adult population in the local area. J Pak Soc Intern Med. 2024;5(2):496–501.
Islam MA, Islam MR, Khan R, et al. Prevalence, etiology and antibiotic resistance patterns of community-acquired urinary tract infections in Dhaka, Bangladesh. PLOS ONE. 2022;17(9):e0274423. https://doi.org/10.1371/journal.pone.0274423
Bhargava K, Nath G, Bhargava A, Kumari R, Aseri GK, Jain N. Bacterial profile and antibiotic susceptibility pattern of uropathogens causing urinary tract infection in the eastern part of Northern India. Front Microbiol. 2022;13:e965053. https://doi.org/10.3389/fmicb.2022.965053
Joya M, Aalemi AK, Baryali AT. Prevalence and antibiotic susceptibility of the common bacterial uropathogens among UTI patients in French Medical Institute for Children. Infect Drug Resist. 2022;15:4291–4297. https://doi.org/10.2147/IDR.S353818
Hrbacek J, Cermak P, Zachoval R. Current antibiotic resistance trends of uropathogens in central Europe: survey from a tertiary hospital urology department 2011–2019. Antibiotics. 2020;9(9):e630. https://doi.org/10.3390/antibiotics9090630
Younas MR, Imran M. Bacterial profile and antimicrobial resistance of uropathogenic Enterobacteriaceae. Urology. 2019;97:24–26
Faine BA, Rech MA, Vakkalanka P, et al. High prevalence of fluoroquinolone-resistant UTI among US emergency department patients diagnosed with urinary tract infection, 2018–2020. Acad Emerg Med. 2022;29(9):1096–1105. https://doi.org/10.1111/acem.14545
Meena P, Rana DS, Bhalla AK, et al. Clinical profile and predisposing factors for the development of urinary tract infection during the first 3 months postrenal transplantation: a tertiary care hospital experience. Indian J Transplant. 2020;14(2):104–110. https://doi.org/10.4103/ijot.ijot_66_19
Jalil MB, Al Atbee MYN. The prevalence of multiple drug resistance Escherichia coli and Klebsiella pneumoniae isolated from patients with urinary tract infections. J Clin Lab Anal. 2022;36(9):e24619. https://doi.org/10.1002/jcla.24619
Dadi BR, Abebe T, Zhang L, Mihret A, Abebe W, Amogne W. Distribution of virulence genes and phylogenetics of uropathogenic Escherichia coli among urinary tract infection patients in Addis Ababa, Ethiopia. BMC Infect Dis. 2020;20(1):e108. https://doi.org/10.1186/s12879-020-4844-z
Girija S, Priyadharsini JV, Paramasivam A. Prevalence of Acb and non-Acb complex in elderly population with urinary tract infection (UTI). Acta Clin Belg. 2021;76(2):106–112. https://doi.org/10.1080/17843286.2019.1669274
Pardeshi P. Prevalence of urinary tract infections and current scenario of antibiotic susceptibility pattern of bacteria causing UTI. Indian J Microbiol Res. 2018;5(3):334–338. https://doi.org/10.18231/2394-5478.2018.0070
Odoki M, Aliero AA, Tibyangye J, et al. Prevalence of bacterial urinary tract infections and associated factors among patients attending hospitals in Bushenyi District, Uganda. Int J Microbiol. 2019;2019(1):e4246780. https:/doi.org/10.1155/2019/4246780
Govindarajan DK, Kandaswamy K. Virulence factors of uropathogens and their role in host pathogen interactions. Cell Surf. 2022;8:e100075. https://doi.org/10.1016/j.tcsw.2022.100075
Fatima T, Rafiq S, Iqbal A, Husnain S. Prevalence and antibiogram of MDR E. coli strains isolated from UTI patients—1-year retrospective study at Nishtar Medical Hospital, Multan. SN Compr Clin Med. 2020;2(4):423–431. https://doi.org/10.1007/s42399-020-00246-8
Bullens M, de Cerqueira Melo A, Raziq S, et al. Antibiotic resistance in patients with urinary tract infections in Pakistan. Public Health Action. 2022;12(1):48–52. https://doi.org/10.5588/pha.21.0071
Acharjee M. Prevalence of urinary tract infection among the patients admitted in the Brahmanbaria Medical College Hospital in Bangladesh. Merit Res J Med Med Sci. 2020;8:111–119. https://doi.org/10.5281/zenodo.3832418
Idrees MM, Rasool MF, Imran I, et al. A cross-sectional study to evaluate antimicrobial susceptibility of uropathogens from South Punjab, Pakistan. Infect Drug Resist. 2022;15:1845–1855. https://doi.org/10.2147/IDR.S356489
Ejaz H, Imran M, Zafar A, et al. Phenotypic Characterisation of Carbapenemase-Producing Escherichia coli Isolated from a Tertiary Care Paediatric Hospital. Int Med Jl. 2020;27(2):e155.
Rizvi ZA, Jamal AM, Malik AH, Zaidi SMJ, Rahim NUA, Arshad D. Exploring antimicrobial resistance in agents causing urinary tract infections at a tertiary care hospital in a developing country. Cureus. 2020;12(8):e9735. https://doi.org/10.7759/cureus.9735
Hasan T. Extended spectrum beta lactamase E. coli isolated from UTI patients in Najaf Province, Iraq. Int J Pharm Res. 2020;17(1):00–00. https://doi.org/10.31838/ijpr/2020.12.04.049
Sendra E, Montesinos IL, Rodriguez-Alarcón A, et al. Comparative analysis of complicated urinary tract infections caused by extensively drug-resistant Pseudomonas aeruginosa and extended-spectrum β-lactamase-producing Klebsiella pneumoniae. Antibiotics. 2022;11(11):e1511. https://doi.org/10.3390/antibiotics11111511
Karruli A, Catalini C, D’Amore C, et al. Evidence-based treatment of Pseudomonas aeruginosa infections: a critical reappraisal. Antibiotics. 2023;12(2):e399. https://doi.org/10.3390/antibiotics12020399
Gajdács M, Ábrók M, Lázár A, et al. Increasing relevance of Gram-positive cocci in urinary tract infections: a 10-year analysis of their prevalence and resistance trends. Sci Rep. 2020;10:e17658. https://doi.org/10.1038/s41598-020-74834-y
Copyright (c) 2025 Muhammad Anees Sharif, Muhammad Imran, Ramna Zia, Ali Hamza, Hashim Ali, Adeel Shahid, Muhammad Ilyas, Areeba Manzoor, Nida Tahir

This work is licensed under a Creative Commons Attribution 4.0 International License.
BSR follows an open-access publishing policy and full text of all published articles is available free, immediately upon publication of an issue. The journal’s contents are published and distributed under the terms of the Creative Commons Attribution 4.0 International (CC-BY 4.0) license. Thus, the work submitted to the journal implies that it is original, unpublished work of the authors (neither published previously nor accepted/under consideration for publication elsewhere). On acceptance of a manuscript for publication, a corresponding author on the behalf of all co-authors of the manuscript will sign and submit a completed the Copyright and Author Consent Form.










